Digital workflow in implant-prosthetic rehabilitation of high aesthetic value sectors: from literature to clinic
Машинний переклад
Оригінальна стаття написана мовою IT (посилання для прочитання).
Today, the digital workflow plays an increasingly important role in dentistry. The advantage of computer-guided or computer-assisted implant surgery (CAI, Computer Aided Implantology) lies in the placement of implants using a surgical guide designed and produced with CAD/CAM technology; this prosthetically guided placement of implants is achieved through the use of software for virtual implant planning. In implant-prosthetic rehabilitations of the anterior sectors using computer-guided surgery, it is possible to correctly position the implants to achieve an optimal aesthetic result. The purpose of this case report is to show the rehabilitation of a maxillary central incisor through immediate computer-guided implant placement with an immediate loading protocol for the prosthesis.
Introduction
The implant-prosthetic rehabilitation of the frontal sectors with high aesthetic value represents a challenge that the clinician must face, knowing perfectly the various therapeutic options available, methodologies that derive from a rigorous and careful examination of the scientific literature.
The pre-implant analysis of aesthetic parameters EIND1 allows to highlight the critical issues of the case and to optimize its realization by identifying the type of implant surgery and the aesthetic result based on the surgical timing (class 1, 2, 3, 4). The 4D positioning, already described in 2007 by the Salama group, highlights how clinical success depends not only on the ideal three-dimensional positioning of the implant in the bone but also on the correct management of the profiles of hard and soft tissues, which often require increments or corrections, and on a proper implant and prosthetic design.
A digital analysis consisting of an intraoral optical impression in the diagnostic phase, an analog or digital diagnostic wax-up, a pre-operative CBCT, and a matching of all this information in a computer-assisted surgery software allows to make the most of the collected information and to perform a prosthetically guided surgery.
Materials and methods
The patient MS, 24 years old, came to our attention in emergency due to the aftermath of a car accident. Upon extraoral and intraoral clinical examination, laceration of the upper lip, partial crown fracture of dental elements 1.2, 1.1, and 2.1, and a horizontal fracture at the middle third of the root of element 2.1 were observed, highlighted by the periapical endoral X-ray performed with a Rinn centering device (Figs. 1-3).



The dental elements 1.1 and 1.2 have been reconstructed (with immediate absence of pulp vitality, to be tested again at 3 and 5 months), while the dental element 2.1, non-recoverable, required extraction.
After a thorough diagnostic evaluation with the clinical examination, which highlighted the absence of periodontal probing that could suggest a fracture of the vestibular cortical bone and with the three-dimensional radiographic examination (Fig. 4), it was decided, in agreement with the patient, to proceed with immediate implant-prosthetic rehabilitation through computer-assisted surgery with immediate loading. The complete photographic set, along with the clinical and radiographic examinations, highlighted the critical issues of the case: young patient, upper central incisor, very high aesthetic demands, thin and scalloped periodontal biotype, root fracture between the middle third and apical third.
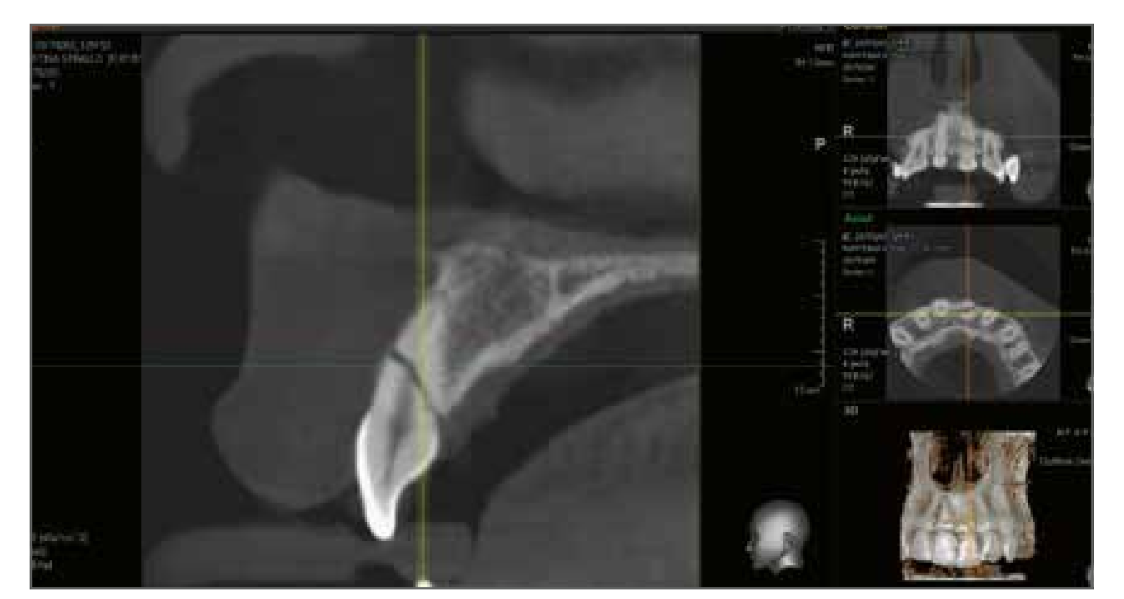
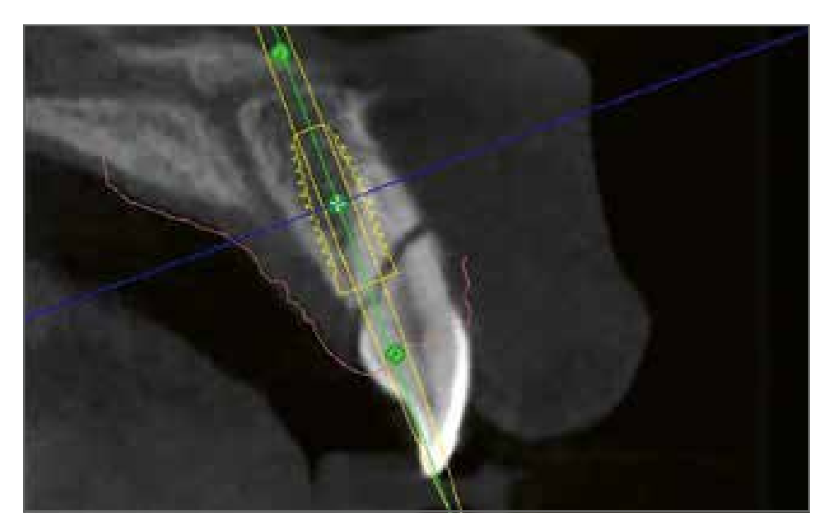
Two digital impressions of the arches were taken, a diagnostic wax-up was made on element 2.1, and a CBCT was performed with the occlusal registration support Navibite (Biomax, Vicenza) which, along with the 2 STL files, were uploaded to the Navimax software to plan the extraction and immediate placement of the implant in relation to the bone crest, the bone margin of the adjacent incisor, and the diagnostic wax-up (Fig. 5). In accordance with the data present in the literature, the placement of a Biomet 3I T3 implant (Biomet, Palm Beach Gardens, Florida, United States) with integrated platform switching 4/3 x 13 mm was planned to be positioned 1.5 mm below the vestibular crestal margin, to be kept intact at the time of tooth extraction. The analysis at Navimax allowed for observation of how the correct implant positioning in the three dimensions of space highlighted in the implant-centric representation the presence of bone at 360°, how primary implant stability could also be sought in the apical portion of the dental socket, and how the prosthetic emergence axis allowed for the management of immediate loading with a screwed provisional. Once the surgical planning was confirmed, the file was sent to the production center for the creation of a dental-supported Navident surgical guide (Fig. 6).

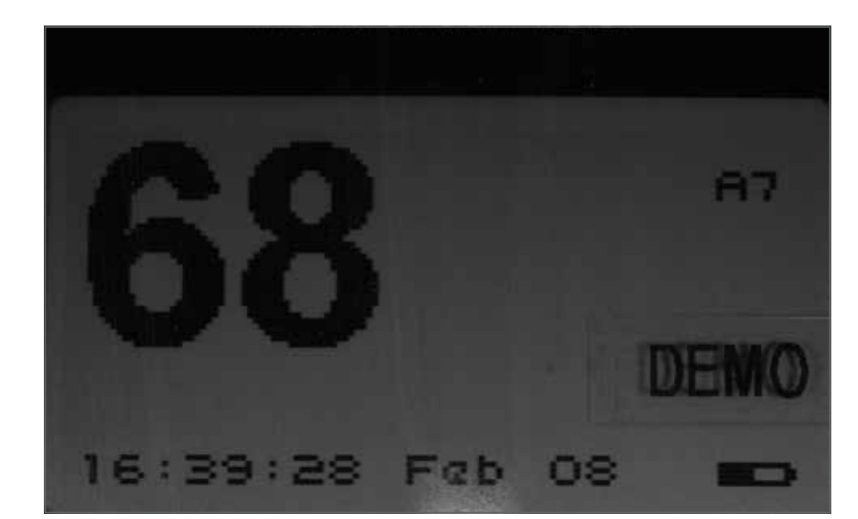
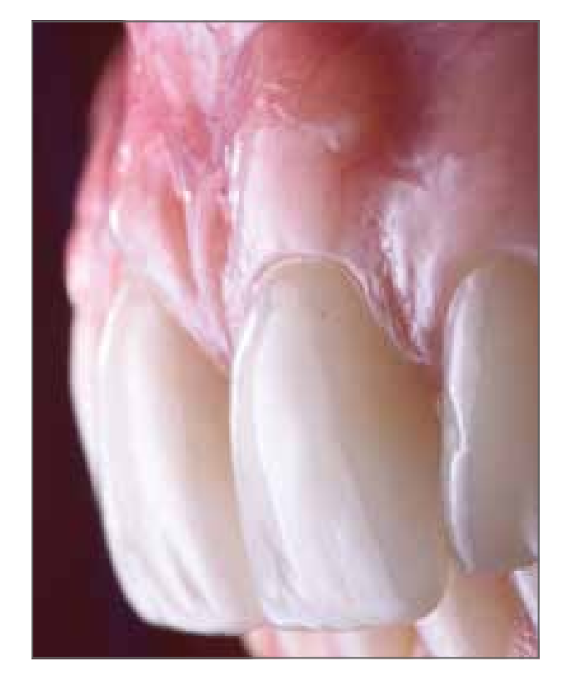
At the time of the surgical intervention (3 days after the accident), following appropriate antibiotic prophylaxis (2 g of amoxicillin and clavulanic acid 1 hour before the intervention) and after plexus anesthesia with articaine 1:100,000, without incision of the mesial and distal papillae, the dental element 2.1 (Fig. 7) was atraumatically extracted with piezoelectric instruments preserving the vestibular cortical bone (essential for managing the immediate post-extraction phase). Once the surgical guide was positioned, the implant site was prepared with the Navigator surgical kit using a sub-preparation technique, and the Biomet 3I T3 4/3 x 13 mm implant was placed as planned (Fig. 8); the insertion torque was above 70 N/cm and the resonance frequency measured with Osstel was 68 ISQ (Fig. 9). The peri-implant gap was managed, in accordance with the data present in the literature5, with deproteinized bovine bone particulate (Bio-Oss granules, Geistlich Biomaterials, Thiene) to counteract the resorption of the vestibular bundle bone. As analyzed in the diagnostic phase, the patient exhibited a thin and scalloped biotype, which made it necessary to increase and stabilize the soft tissues on one side with a platform switching implant, in order to have more space to achieve soft tissue stability, and on the other side with a connective graft inserted as a partial thickness vestibular envelope. The graft was taken from the palatal region, following anesthesia of the surrounding area with articaine 1:100,000, with a rectangular epithelial-connective incision of 1.5 mm thickness, approximately 4 mm height, and a length equal to the area to be treated, of about 10 mm (Fig. 10).



After suturing the donor site, the graft was de-epithelialized, leaving a connective thickness of about 1.2 mm, which was positioned, after the partial thickness vestibular flap incision at element 2.1, 1 mm above the bone crest and sutured with a resorbable Vicryl 6-0 suture, in such a way as to achieve a thickness of the vestibular flap between 2.5 and 3 mm, as highlighted in the works of Zucchelli et al.6 (Fig. 11). The provisional obtained from the diagnostic wax-up was then positioned and relined in the mouth with the aid of a repositioning prosthetic template. The subgingival profile of the provisional was maintained concave without compressing the vestibular tissues, in order to leave the crestal space for the maturation of the soft tissues. The mesial and distal contact points were managed according to the indications of Tarnow et al.7,8 to achieve complete reformation of the interproximal papillae (Fig. 12). Furthermore, the provisional was uncoupled in the contacts in centric, protrusive, and lateral movements. The patient was discharged with supportive pharmacological therapy and was recalled for clinical and joint checks at 2 weeks (suture removal), 4, 8, 12, and 16 weeks, observing the maturation of the soft tissues and radiographic bone healing.


At 4 months, with the continued absence of vitality of element 1.1, root canal therapy was performed, reconstruction with a fiberglass post, and placement of a provisional resin crown.
The removal of the provisional screw-retained on the implant, 4 months after the surgical intervention, allowed for the perfect integration of the connective graft and the vascularization of the site with circumferential and perpendicular connective fibers (Fig. 13); the new resonance frequency level had increased to 80 ISQ.

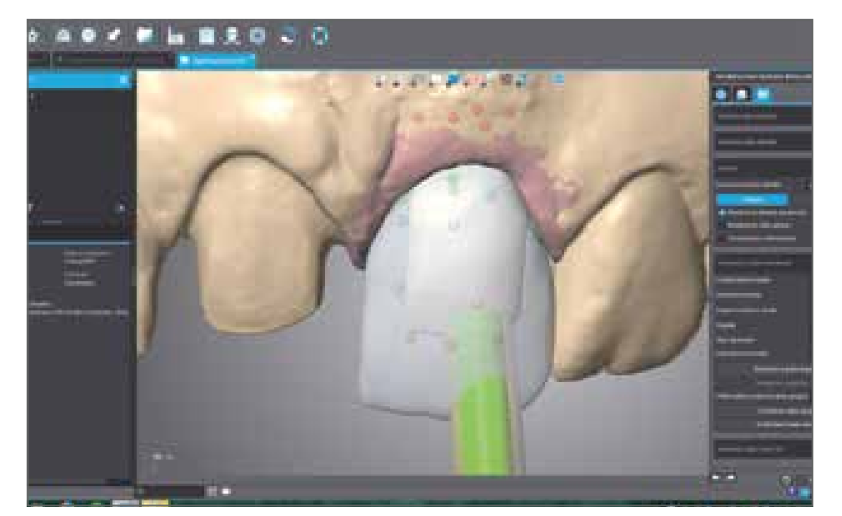
The finalization of the case involved the use of a digital impression technique with the Carestream 3600 intraoral optical scanner (Carestream Health, Rochester, New York, United States). According to the correct digital protocol, the optical impression of the maxillary arch was obtained with the provisional restorations in place, the extraoral impression of the individual provisional restorations, the impression of the properly prepared natural tooth with Ultrapack 00 retraction cord (Ultradent Products Inc., Salt Lake City, Utah, United States) and modified chamfer preparation, the impression of the transmucosal pathway obtained from the implant site, and the impression of the implant positioning with the scan body (Figs. 14,15). Finally, the impression of the opposing arch and the occlusal registration check were obtained.


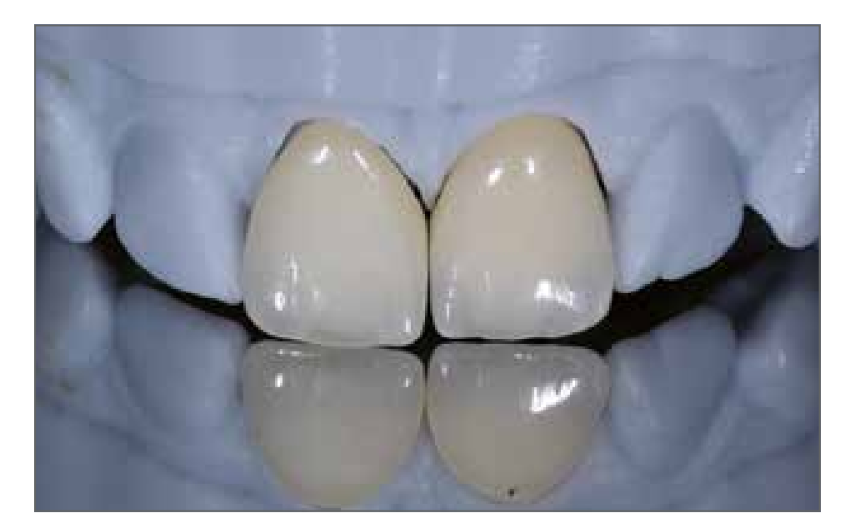
The laboratory phases, also carried out with an almost completely digital workflow, involved the creation of a zirconia implant abutment using the bonding technique, with a concave subgingival profile, and 2 layered zirconia-ceramic crowns: hence the need to also have a polyurethane working model that allowed for the correct layering of the ceramic to achieve excellent aesthetics that could satisfy the patient, the clinician, and the dental technician (Figs. 16-18). The conditioning of the soft tissues on element 2.1 was ideal and allowed, after tightening the zirconia abutment to 25 N/cm and the adhesive cementation of the two crowns, to achieve optimal aesthetics and camouflage of the two central incisors (Figs. 19-22).




The three-dimensional radiographic examinations confirm the result obtained (Figs. 23, 24). The 24-month follow-up showed optimal aesthetic results with stabilization of hard and soft tissues (Fig. 24).


Discussion
The ability to virtually plan the placement of dental implants and position them in the exact three-dimensional location within the alveolar bone, through appropriately milled or 3D printed surgical templates, has long been a reliable and predictable clinical reality. In fact, guided surgery has been considered a successful clinical procedure for over 10 years, as evidenced by various clinical studies and systematic reviews of the literature.
Furthermore, the introduction of technologies for digital image acquisition has completely revolutionized the workflow. Firstly, the introduction of Cone Beam Computed Tomography (CBCT), which allows for the acquisition of 3D information about the bone anatomy with a low radiation dose for the patient and high image quality. Secondly, the introduction of increasingly accurate and high-performing intraoral optical scanners has represented a further evolution in image acquisition techniques for surgical planning. In fact, thanks to such machines, it is possible to acquire all the necessary information related to hard and soft tissues simply, precisely, and accurately, through a simple beam of light. Moreover, when defects or deficiencies in the image are noticed, it is possible to re-capture only the small area where the error was highlighted, without the need to redo the entire impression, as is the case with analog impressions.
These new technologies have allowed, by processing the data and information obtained with dedicated software, to improve pre-surgical planning, simulating both the surgical phase and the prosthetic phase, but they have also enabled the production center to create a surgical guide supported by dental structures.
It is evident how numerous the advantages are of transitioning from an analog workflow to a digital one, including: better diagnosis and treatment planning, with the possibility to study and plan therapies in detail and in 3D, whether they are prosthetic, surgical, or orthodontic; quality control of production processes, with standardization at optimal levels of prosthetic restorations made from highly aesthetic materials; in surgery, safety increases through guided implant placement (possibility of a full-digital workflow) and the use of custom-made titanium grafts and meshes, tailored to the patient's defect; cost reduction, related not only to production processes but also to consumables (reduction of the need for traditional impression materials, no shipping costs since files are sent electronically); reduction of treatment times, as appointments are significantly reduced, saving time for both the clinician and the patient; less stress for the patient during the impression-taking procedures using the intraoral scanner; high-quality perception from the patient, with whom it is possible to communicate directly, showing high-quality 3D images of the various surgical and prosthetic phases, making it easier for them to accept the costs associated with even complex treatments.
Despite the multiple advantages, there is still not a high diffusion of the digital workflow today, probably due to the following reasons: apparent complexity of the protocols and their application; learning curve; startup costs related to the purchase of equipment and annual software upgrades; costs of individual devices (dental models and dedicated surgical kits).
However, with the increasing presence in the market of a growing number of companies specialized in the digital sector, there has been an increase in supply and competition, leading to a significant reduction in prices. Consequently, both the software and the entire workflows have been greatly simplified, making them more accessible to clinicians.
Conclusions
The implant-prosthetic rehabilitation of a central incisor in a young patient represents a great challenge and commitment for the clinician: the digital technology available today, which starts from a three-dimensional examination of the jawbones and dental arches, from a digital analysis of the smile with wax-up and leads to the realization of computer-guided implant surgery with immediate prosthetics, allows for the optimization of the workflow and achieves, in accordance with the data present in the scientific literature, functional and aesthetic results.
Filippo Tomarelli, Giuseppe Marano, Maurizio De Francesco, Giorgio Serafini
Bibliography
- Dursun E, Lin GH, Taheri S, Chu SJ, Wang HL, Tözüm TF. A Comparison of Esthetic Features of Pre-existing Natural Tooth Versus Post-Implant Restoration in the Esthetic Zone: A Retrospective 12-month Follow-up. Int J Oral Maxillofac Implants. 2018 Jul/Aug;33(4):919-928.
- Funato A, Salama MA, Ishikawa T, Garber DA, Salama H. Timing, positioning, and sequential staging in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007 Aug;27(4):313-23.
- Grunder U. Crestal ridge width changes when placing implants at the time of tooth extraction with and without soft tissue augmentation after a healing period of 6 months: report of 24 consecutive cases. Int J Periodontics Restorative Dent. 2011 Feb;31(1):9-17.
- Chen ST, Buser D. Esthetic outcomes following immediate and early implant placement in the anterior maxilla-a systematic review. Int J Oral Maxillofac Implants. 2014;29 Suppl:186-215.
- Chu SJ, Salama MA, Garber DA, Salama H, Sarnachiaro GO, Sarnachiaro E, Gotta SL, Reynolds MA, Saito H, Tarnow DP. Flapless Postextraction Socket Implant Placement, Part 2: The Effects of Bone Grafting and Provisional Restoration on Peri-implant Soft Tissue Height and Thickness- A Retrospective Study. Int J Periodontics Restorative Dent. 2015 Nov-Dec;35(6):803-9.
- Zucchelli G, Gori G, Mele M, Stefanini M, Mazzotti C, Marzadori M, Montebugnoli L, De Sanctis M. Non-carious cervical lesions associated with gingival recessions: a decision-making process. J Periodontol. 2011 Dec;82(12):1713-24.
- Jung RE, Heitz-Mayfield 2, Schwarz F; Groups of the 2nd Osteology Foundation Consensus Meeting. Evidence-based knowledge on the aesthetics and maintenance of peri-implant soft tissues: Osteology Foundation Consensus Report Part 3-Aesthetics of peri-implant soft tissues. Clin Oral Implants Res. 2018 Mar;29 Suppl 15:14-17.
- Tarnow D, Elian N, Fletcher P, Froum S, Magner A, Cho SC, Salama M, Salama H, Garber DA. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003 Dec;74(12):1785-8.
- Testori T, Robiony M, Parenti A, Luongo G, Rosenfeld AL, Ganz SD, Mandelaris GA, Del Fabbro M. Evaluation of accuracy and precision of a new guided surgery system: a multicenter clinical study. Int J Periodontics Restorative Dent. 2014;34 Suppl 3:s59-69.
- Van Assche N, Vercruyssen M, Coucke W, Teughels W, Jacobs R, Quirynen M. Accuracy of computer-aided implant placement. Clin Oral Implants Res. 2012 Oct;23 Suppl 6:112-23.
- Daas M, Assaf A, Dada K, Makzoumé J. Computer-Guided Implant Surgery in Fresh Extraction Sockets and Immediate Loading of a Full Arch Restoration: A 2-Year Follow-Up Study of 14 Consecutively Treated Patients. Int J Dent. 2015;2015:824127.
- D’haese J, Van De Velde T, Komiyama A, Hultin M, De Bruyn H. Accuracy and complications using computer-designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: a review of the literature. Clin Implant Dent Relat Res. 2012 Jun;14(3):321-35.
- Ganz SD. Three-dimensional imaging and guided surgery for dental implants. Dent Clin North Am. 2015 Apr;59(2):265-90.
- Al-Okshi A, Lindh C, Salé H, Gunnarsson M, Rohlin M. Effective dose of cone beam CT (CBCT) of the facial skeleton: a systematic review. Br J Radiol. 2015 Jan;88(1045):20140658.
- Dawood A, Brown J, Sauret-Jackson V, Purkayastha S. Optimization of cone beam CT exposure for pre-surgical evaluation of the implant site. Dentomaxillofac Radiol. 2012 Jan;41(1):70-4.
- Zimmermann M, Mehl A, Mörmann WH, Reich S. Intraoral scanning systems - a current overview. Int J Comput Dent. 2015;18(2):101-29.
- Ting-Shu S, Jian S. Intraoral Digital Impression Technique: A Review. J Prosthodont. 2015 Jun;24(4):313-21.
- Yuzbasioglu E, Kurt H, Turunc R, Bilir H. Comparison of digital and conventional impression techniques: evaluation of patients’ perception, treatment comfort, effectiveness and clinical outcomes. BMC Oral Health. 2014 Jan 30;14:10.
- Patzelt SB, Lamprinos C, Stampf S, Att W. The time efficiency of intraoral scanners: an in vitro comparative study. J Am Dent Assoc. 2014 Jun;145(6):542-51.

/social-network-service/media/default/101731/b396a315.jpg)