Tissue Engineering in Temporomandibular Joint Reconstruction
Introduction
Temporomandibular joint (TMJ) reconstruction presents many challenges. Care must be taken when designing study protocols to avoid erroneous or dubious results. It is also imperative to choose correctly the type of animal to include in the studies. Failures from the past, using silicone and teflonbased materials in TMJ, have been key lessons for the future. The gradual growth of tissue engineering (TE) can be a promising field for emerging TMJ biomaterials if basic principles are respected to achieve safe and effective solutions for TMJ.
Animal model for temporomandibular joint tissue engineering
To improve human health, scientific discoveries and technologies must be translated into practical applications. Such advances classically begin with basic research and then progress to the clinical level. Inherent to the development of new technologies is the role of preclinical trials using animal models. Although no animal model can fully replicate human conditions, animal models are key for the evaluation of mechanisms of disease, testing new technologies, applying new procedures and progress of TE.
The absence of a well-established animal model for TMJ investigation has been a limiting factor for the potential progress of TMJ TE. The choice of an animal for experimental design is not straightforward, mostly because of physiologic and anatomic differences. TMJ is a cardinal feature that defines the class Mammalia and separates mammals from other vertebrates. TMJ shows remarkable morphologic and functional variation between different species, reflecting not only the great mammalian adaptation to feeding mechanisms but also different biomechanical behavior. The morphologic variations are mostly correlated to loading (eg, size of articular surfaces) or movement (eg, orientation of the joint), or both. Loading of the TMJ is a reaction force arising from the contraction of the masticatory muscles; its magnitude depends strongly on the position of the bite point relative to the muscle action line. Many preclinical studies used laboratory animals, especially rodents; however, they fall into the category of minimal TMJ loading, especially during chewing. In contrast, carnivores, such as dogs, sustain TMJ loads that are higher than those of primates. Opening of the jaw usually involves a combination of rotation and forward sliding (translation), but some carnivores have lost the ability to slide, and some specialized anteaters instead use a rotation around the long axis of the curved mandible. The most extreme evolutionary variants include loss of the synovial cavity in some baleen whales; loss (or possibly primitive absence) of the disc in monotremes, some marsupials, and edentates (anteaters and sloths); variations in the orientation of the joint cavity from sagittal (many rodents) to transverse (many carnivores); reversal of the usual convex/concave relation so that the processus condylaris becomes the female element (many artiodactyl ungulates such as sheep and cattle). In addition, the size of the joint is extremely variable. Pig, sheep, rabbit, and monkey have been used as TMJ disc defect models in many studies. The monkey model is barely used in recent years, considering the high cost, difficult surgical operation, and ethical approval. The rabbit is often used as a model for disc displacement studies. However, the same limitations are present in the rabbit: (1) the small size of the TMJ, increasing the difficulty for surgical approach; (2) the zygomatic arch sometimes needs to be removed to access the joint; (3) the TMJ loading is reduced, causing a possible bias in the results. The most cited study of a TMJ disc displacement model used adult male New Zealand white rabbits to surgically induce anterior disc displacement. The procedure required an incision above the zygomatic process and fracture of the zygomatic process of the squamous temporal bone to access the joint. The surgical approach alone could have an impact on the results and is a limitation of this model.
One of the main reasons that larger animals, rather than mice, rats, and rabbits, are commonly used for the study of TMJ surgical methods is the adequate surgical access and adequate TMJ loading, increasing the accuracy of possible mechanical testing. For that reason, mice, rats, and rabbits present technical challenges that frequently raise questions regarding the translational relevance to the human TMJ, justifying why those animals are not recommended for rigorous preclinical trials for TMJ TE.
In the large animal section, historically, the pig has been regarded as the gold standard, based on general similarities to the human anatomy, specifically, the size of the articular TMJ structures and the shape of the disc. Furthermore, a recent comprehensive study has validated the use of the Yucatan minipig as an animal model for TMJ TE studies. However, the zygomatic arch shields the joint space in the farm pig, representing, in the authors’ opinion, a limitation for the use of this model. Moreover, the biomechanical forces of the minipig can compromise the results.
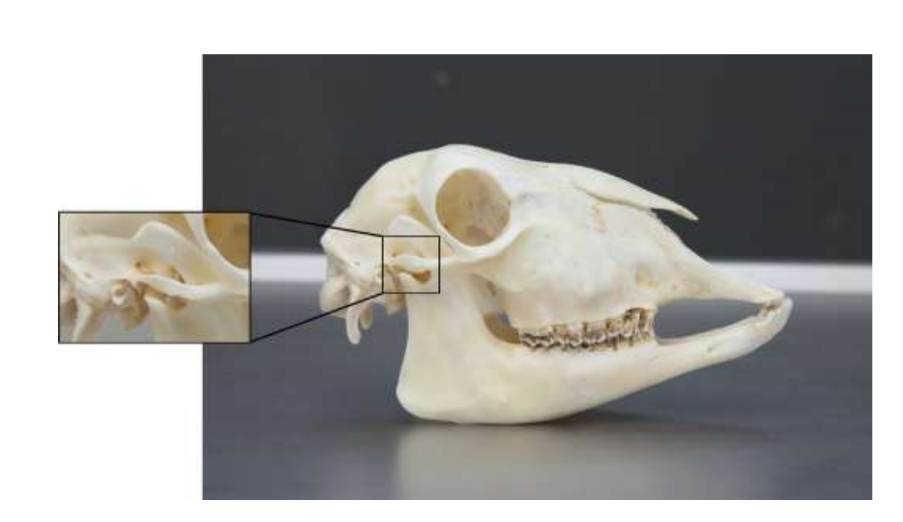
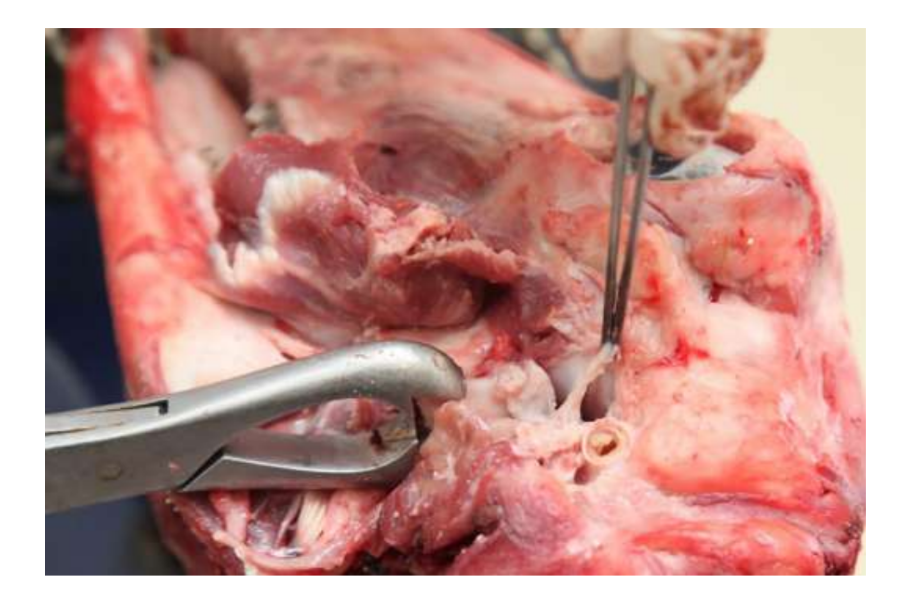
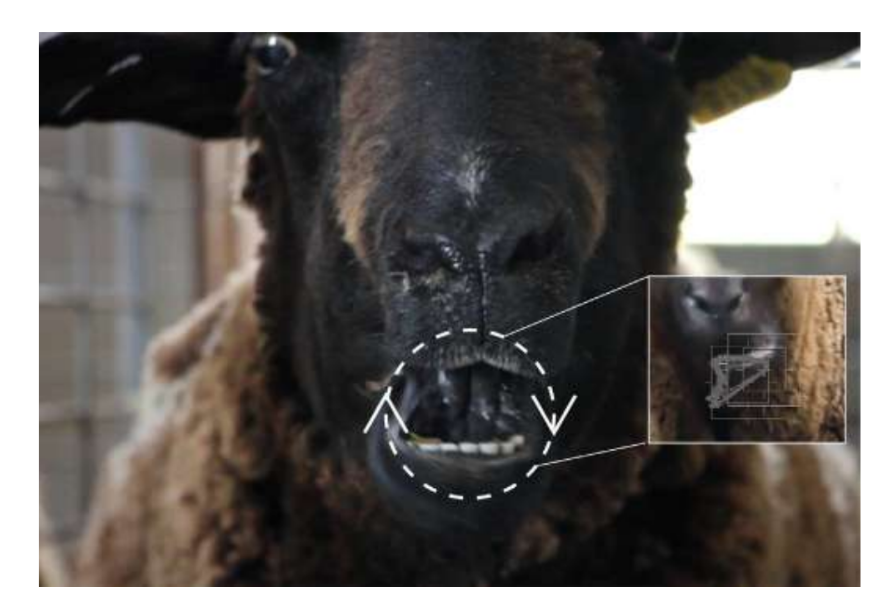
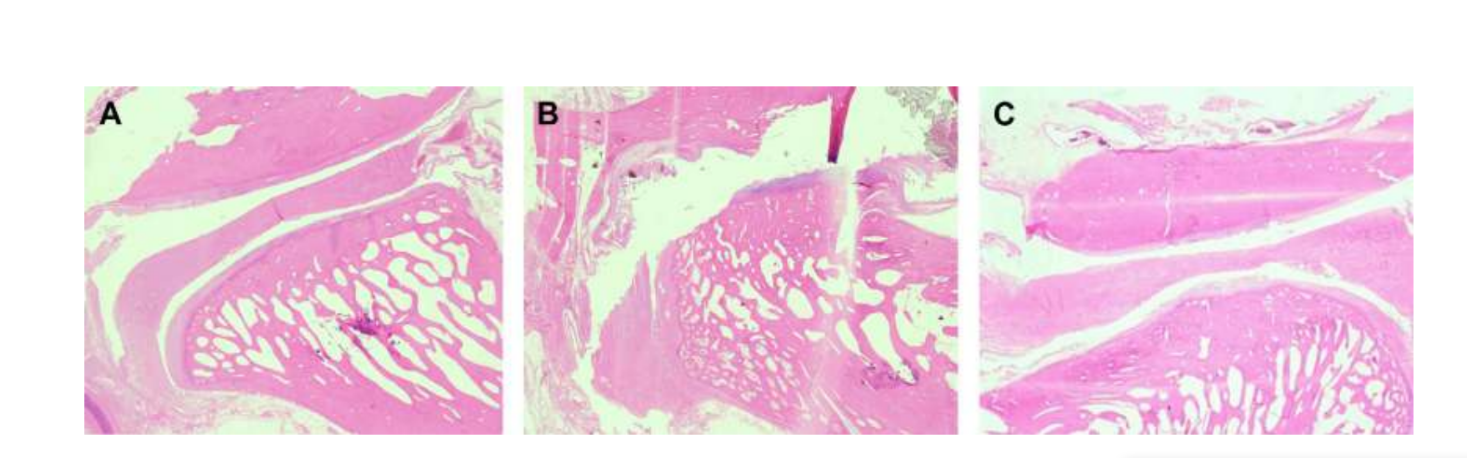
The TMJ anatomy, histology, and biomechanics of black Merino sheep have been also studied (Fig. 1). With a preauricular incision and blunt dissection, the TMJ capsule can be easily accessed (Figs. 2 and 4), even for TMJ arthrocentesis. One advantage is the zygomatic arch does not shield the joint space, as is the case in the farm pig. The TMJ disc separates the upper from the lower compartment (Fig. 3 and 4). The sheep’s condyle is mediolaterally concave with ellipsoidal shape and with the longer axis in the mediolateral position (Figs. 5 and 6). These anatomic similarities to human TMJ, associated with the large experience in in-vivo TMJ surgical investigation, suggest the sheep can be considered a suitable model to conduct rigorous TMJ surgical investigation.




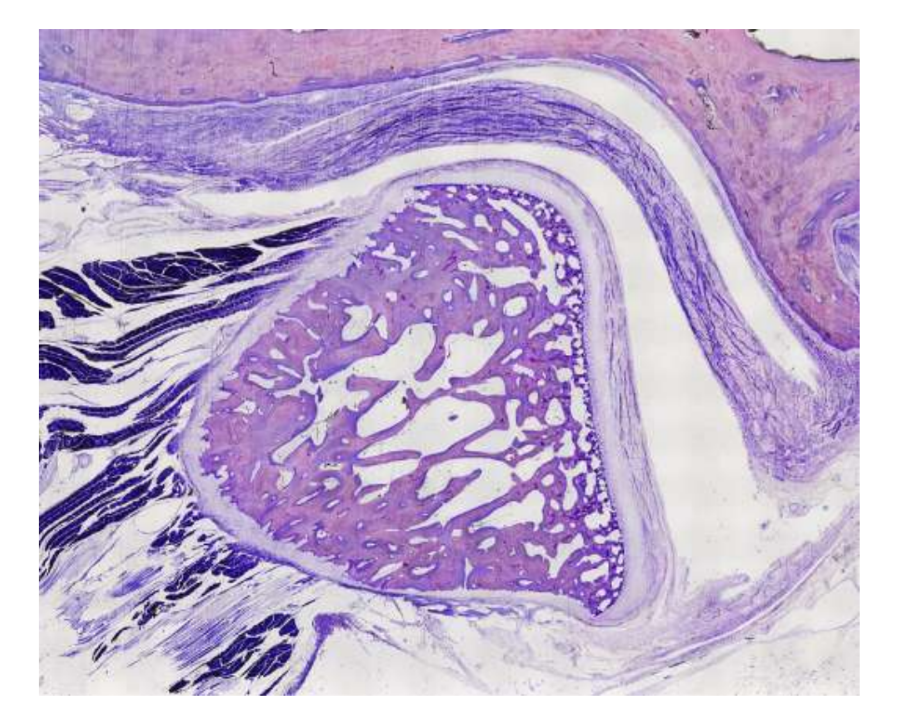
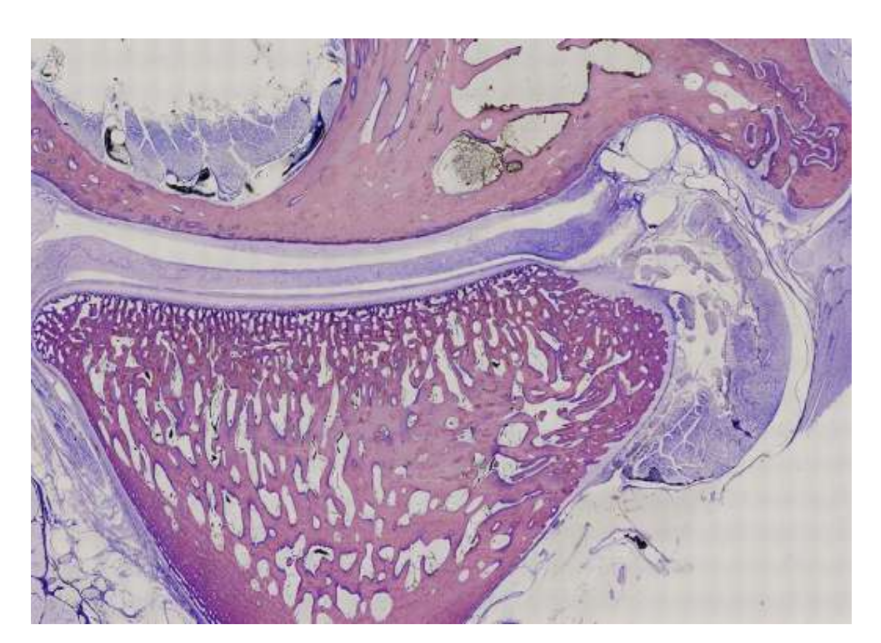
Sheep are a valid option for TMJ studies considering the TMJ size, processus condylaris and fossa mandibularis shape, disc size, morphology, and attachments. The histology analysis has a great resemblance to human TMJ (Figs. 7 and 8). Another important advantage regarding the sheep model is the rumination process (Fig. 9), providing additional biomechanical loading in the TMJ, ideal to test in-vivo TE material resistance. Recently, the sheep animal model was successfully used in a preclinical TMJ alloplastic reconstruction study.
Although no species provides the gold standard for all preclinical TMJ TE studies, sheep have emerged as a leading option. The minipig and farm pig can be considered when adequate resources are available, serving as acceptable alternatives.
Study design for preclinical temporomandibular joint tissue engineering
The absence of efficacious options to substitute the TMJ disc can be related to difficulties in the translation of animal evidence to the clinical practice in humans. These limitations are likely related to the following:
- The use of heterogeneous animal models with conflicting results, possibly owing to variable anatomy and intra-articular loading between species;
- The use of the contralateral TMJ as control, which may be associated with contralateral overloading;
- The biomaterials used to replace the disc, which do not account for the morphologic and biomechanical characteristics of the native TMJ disc;
- The absence of randomized controlled trials with blinding of outcomes’ assessors;
- The lack of multidisciplinary teams involved in the project.
Preclinical research should promote the effective translation of knowledge into practice. The previously mentioned aspects can limit the effective translation of quality scientific knowledge into clinical practice, and these may present potential issues to patients, clinicians, and scientific progress.
The contemporary absence of successful options to substitute the TMJ disc is still a major issue for public health. Little has changed in the past decade regarding study designs for TMJ investigation, and the treatment of patients with severe temporomandibular disorders (TMD) remains controversial. For these reason, future studies need to be rigorous in the study design, respecting the ARRIVE guidelines. TEMPOJIMS is a rigorous preclinical study, with the protocol publicly available. The primary outcome should be the histopathologic analysis. For that, the authors recommend carefully removing the TMJ block as shown in Fig. 10. The histologic preparation is challenging, but the protocol is well detailed by our group, most of the difficulty is in the decalcification process. The study protocol has been used in TEMPOJIMS phase 1: comparing the results of TMJ discectomy versus TMJ discopexy versus TMJ sham surgery, obtaining a baseline for interpretation of future TMJ disc TEresults.

The rationale for temporomandibular joint tissue engineering
To justify TE investigation in TMJ,is necessary to demonstrate the clinical need for a TMJ disc substitute. As far as is known, TMJ discectomy is associated with favorable long-term results, so why invest time and resources in a TMJ disc substitute?
Probably, because, besides the strong evidence, some results on discectomy are conflicting. In previous preclinical studies in this field, the investigators have used the contralateral unoperated side as a control and debatable animal models. Using the contralateral side as a control can be inappropriate considering the contralateral overload impact. Theoretically, a bilateral approach could reduce the bias. The animal variability in the different studies is a warning about the importance of using the same animal model in further studies regarding TMJ TE. Therefore, the authors’ group performed diverse preclinical studies in black Merino sheep, but the first study was to understand the need for a TMJ disc substitute, using a sham surgery control group - TEMPOJIMS phase 1.
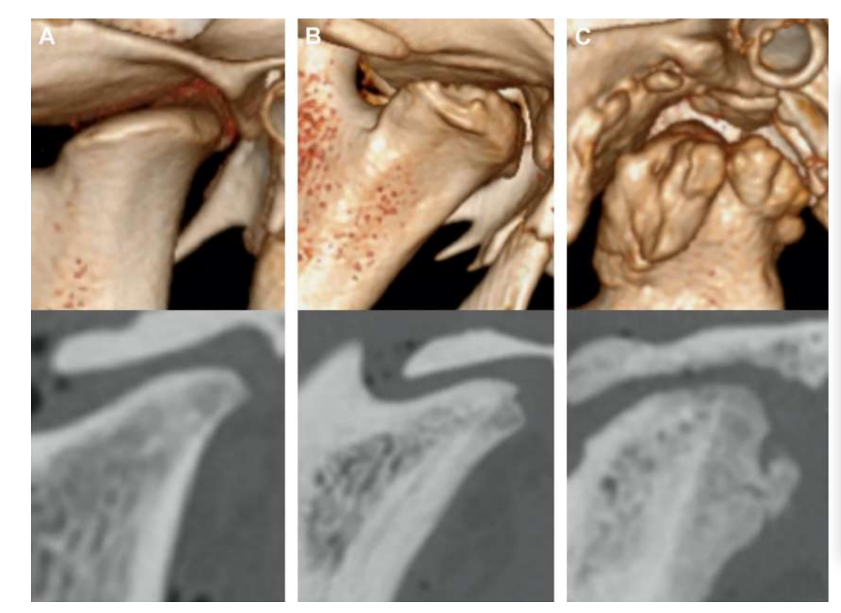
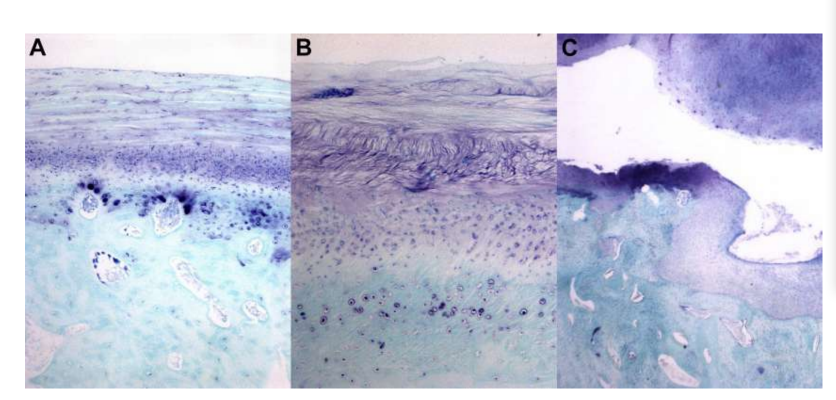
Bilateral TMJ discectomy in black Merino sheep was performed, and severe TMJ changes were detected with both histopathologic and imaging analysis (Figs. 11 and 12). In the postmortem macroscopic evaluation, a severe degenerative process was observed (Fig. 13). In histologic analysis, the investigators verified an increase in proteoglycan and rounded cells and thickening of the cartilage after discectomy. A more severe synovitis in discectomy was also observed, indicating a possible inflammation process. Structurally, differences were detected in shape, condyle sclerosis, temporal sclerosis, condyle marrow, temporal erosion, condyle erosion, and temporal marrow (Fig. 14). However, discectomy had only an effect in absolute masticatory time, rumination time per cycle, and rumination area in first 2 months, and after the initial period no significant changes were noticed. In Macaca fascicularis, Yaillen and colleagues after unilateral discectomy described ankylosis between the condyle and temporal bone. In clinical studies, af Björkesten and Boman in 1947 were the first investigators to report radiographic morphologic changes caused by discectomy, describing “flattening off the articular surface.” In the 1980s, severe condyle flattening and sclerosis in postdiscectomy patients were described. Later, Eriksson and Westesson in a review of 52 patients verified also that most of the joints showed radiographic evidence of osteophytes, flattening, and sclerosis.
Bjørnland and Larheim described fibrous ankylosis 6 months after unilateral discectomy. Together, these results highlighted the importance of studying an effective interposal material to substitute the TMJ disc.
Tissue-engineered implants
The attempt to replace the TMJ disc began being studied around the middle of the 1960s and 1970s. The first materials tested were silicone rubber (Dow-Corning, Midland, MI, USA) and Proplast-Teflon (Vitek, Inc, Houston, TX, USA). Silicone rubber was introduced by Robinson in 1968, in the areas of aesthetic surgery, joint replacements, and oral and maxillofacial reconstructive surgery. Although this material presents interesting properties of easy handling and good resistance and elasticity, its use was quickly discouraged. Some patients presented severe immune reactions, such as reactions against silicone particles and synovitis. Silicone disc substitute was also associated with migration of this material into adjacent tissues. In sheep, the implantation of a sheet of silastic (silicone rubber implant) was responsible for a bone destruction in all 4 operated joints and accompanied for a foreign-body reaction throughout the fibrous tissue capsule that had formed around the implant. Also, Sanders and colleagues in a re-evaluation of 30 patients reported a fibrous capsule as a pseudodisc and a fibrous barrier between the condyle and the fossa.
Proplast-teflon (polytetrafluoroethylene or PTFE) was also another material used as a substitute for the TMJ disc. Introduced in 1976 by Dr Charles Homsy, it was presented as a stable and porous material that allows cell adhesion. However, this material was quickly wearing out, inducing severe reactions, including foreign body granulomas, fibrosis, morphologic alterations of the condyle, and pain. In 1990, the Food and Drug Administration recommended removing these implants in cases whereby degenerative changes in the TMJ were observed.
In view of the consequent failures of these replacement materials, TE has been gaining importance, representing a possible viable route to TMJ disc replacement. An effective and safe articular disc must meet some criteria, such as the following:
- Biodegradability to allow a replacement by a suitable tissue and biocompatibility with the host, to avoid an inflammatory response;
- High load-bearing capacity to withstand the mechanical forces applied;
- Suitable porosity and surface chemistry for cell differentiation and to allow the transport and exchange of oxygen, nutrients, and waste.
In this context, the authors characterized the morphologic, histologic, and biomechanical characterization of the black Merino sheep TMJ disc (Fig. 15). The results of this study were extremely relevant for understanding the geometry and biomechanical and biological properties of the articular disc in order to be able to develop replacement materials. In fact, the great challenge of TE has been to develop a strategy in which a biomaterial contains all these characteristics. In the case of the TMJ, the studies have focused on 2 types of biomaterials: synthetic and natural.
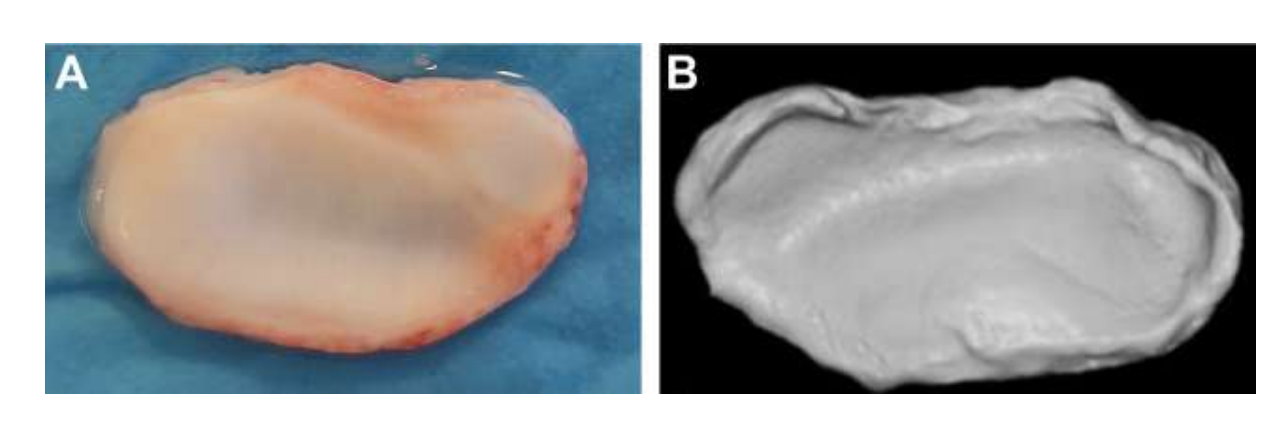
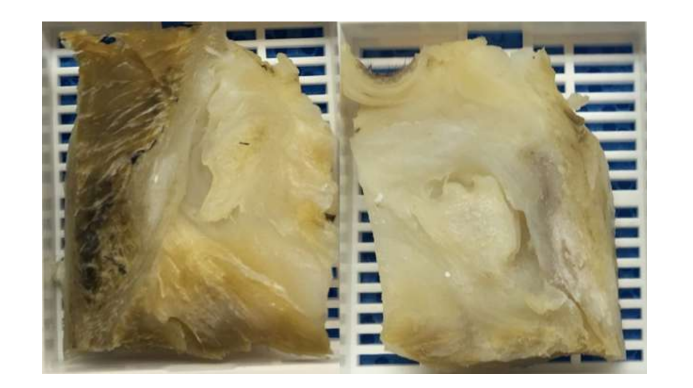
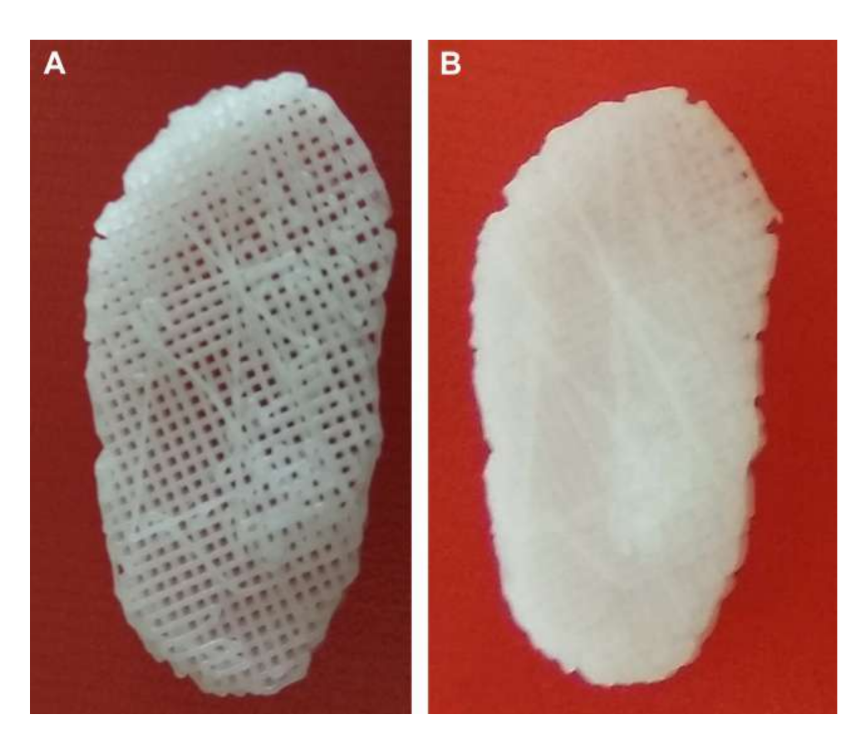
The natural biomaterials are derived from natural sources and present best biological properties, such as biocompatibility, biodegradability, and bioactivity, and promote cell adhesion, proliferation, and differentiation, essential for TE. However, they usually have worse mechanical properties and more difficulty in material processing. Owing to these difficulties, few studies have yet demonstrated the potential use of these biomaterials in TMJ. The first pilot study used fibrin/ chitosan hybrid combined with TMJ synovial stem cells. The investigators showed a promotion of extracellular matrix deposition with the implantation of the scaffold in mice. Despite these promising results, the study did not move forward, and much of this may have been owing to the finging that, after day 7 of cell seeding, the number of cells started to decrease drastically. In another study, a combination of collagen sponge scaffold and autologous bone marrow mesenchymal cells was evaluated in perforated TMJ discs of Japanese rabbits. The investigators observed the formation of new connective tissue after 2 weeks, whereas in control after 8 weeks, the perforation had still not completely closed. However, as already mentioned, the use of rabbits/mice in this type of study has many limitations. Alginate was also studied in an in vitro approach with TMJ disc cells, but the results were not promising, and collagen or GAG formation was not verified, and cell number population decreased in time. Another strategy that has been explored is decellularized extracellular matrix (dECM). dECM has great properties, preserving the native organic and mechanical properties, such as the collagen network of the tissue, as the immunogenic components are removed to allow cell adhesion and proliferation. Few studies have focused on the best method for the effective decellularization of the TMJ disc. More recently, an injectable hydrogel based on decellularized porcine TMJ discs was produced and injected into a mouse. The hydrogel showed good cytocompatibility, and only a minor inflammation was observed within 7 days after implantation. However, this study lacks verification of therapeutic effectiveness. The investigations related to the most effective protocol of decellularizing the disc are scarce. Thus, the authors’ research group is currently extensively studying other methods of decellularization of the black Merino TMJ discs (Fig. 16), such as chemical, physical, and enzymatic, in order to find the most effective strategy.
Synthetic biomaterials compared with natural materials have disadvantages in the structural differences compared with native tissue and possible complications associated with toxicity and biocompatibility. However, they presented some relevant advantages, such as higher availability, easier processing, and better biomechanical and physical properties. For these reasons, synthetic materials are being explored for TMJ disc substitutes.
Polylactide (PLA), which has a longer degradation time, was one of the first synthetic materials studied. The PLA in combination with adipose stem cells increased the expression of aggrecan and collagen type I and II in a chondrogenic medium, but the differentiation degree of the cells was lower when compared with cells derived by the TMJ disc.
Poly(glycolic acid) (PGA) is also a polymer biodegradable studied in the TMJ field. Porcine TMJ disc cells were seeded to a PGA scaffold, and an increased amount of matrix production was verified. Other investigators hypothesized that poly-L-lactic acid (PLLA) nonwoven meshes would limit contraction, allow for comprehensive mechanical evaluation, and maintain viability relative to PGA nonwoven mesh controls. These latter constructs had the capability of maintaining their volume for
6 weeks, when compared with PGA, but presented low mechanical capacity. Poly(ε-caprolactone) (PCL) is another biomaterial that has been studied owing to their slow degradation. PCL scaffolds, where fiber orientation represented the collagen network, have been encapsulated with microspheres
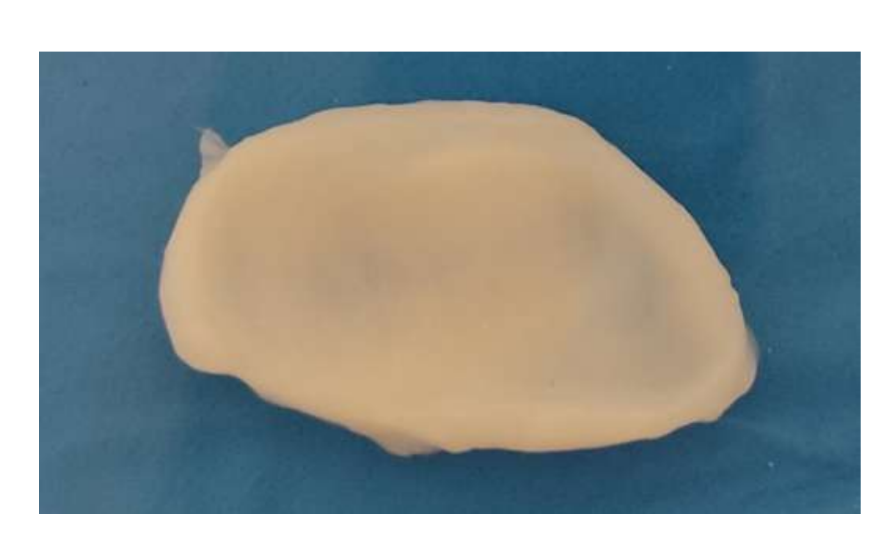
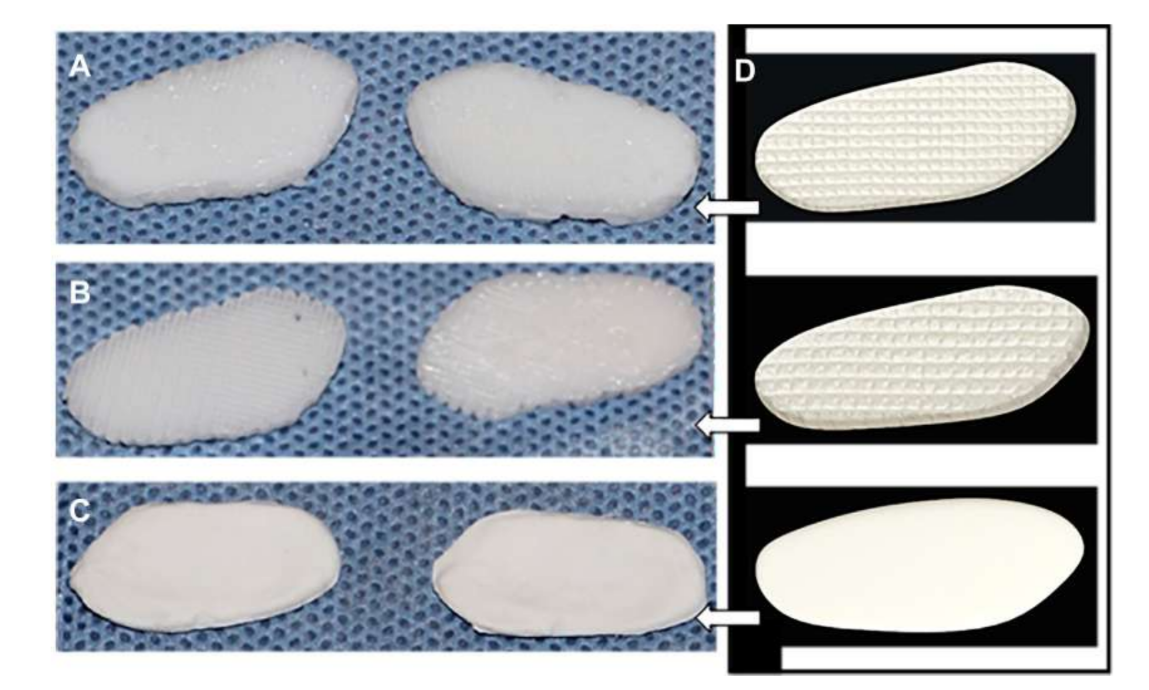
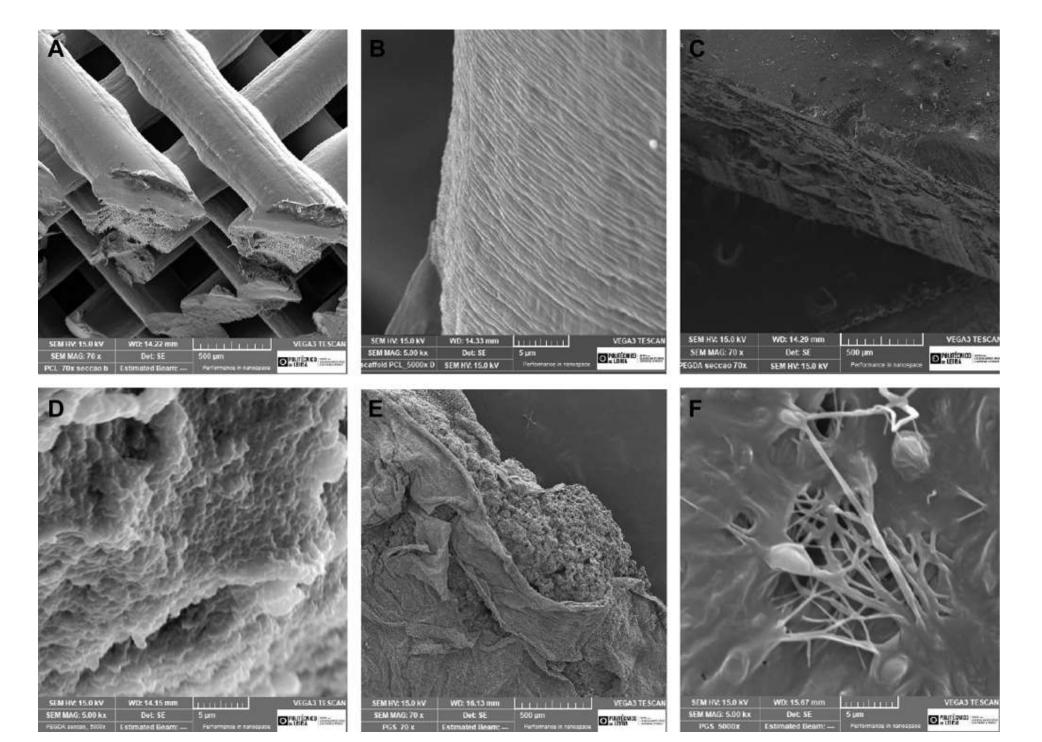
of connective tissue growth factor (CTGF) and transforming growth factor beta 3 (TGFb3). When cultured with human mesenchymal stem/progenitor cells, this scaffold was efficient in generating heterogeneous fibrocartilaginous matrix, and viscoelastic properties. The investigators state that in vivo and long-term scaffold degradation tests must be performed. Jiang and colleagues studied polyvinyl alcohol hydrogel crosslinked by cyclic freeze-thaw and reinforced by 3-dimensional (3D) PCL and implanted in goats for 12 weeks. The investigators described this substitute with an ability to maintain joint stability and protect condylar cartilage and bone from damage. However, it was also reported as an ingrowth of fibrous tissue at the surrounding area of PCL. In fact, PCL does not seem to have the ideal properties to be used as a substitute in the works that have been done. The authors’ research group also studied biomaterials based on scaffolds and hydrogels mimicking the TMJ disc of black Merino sheep, using different materials, PCL and polyethylene glycol diacrylate (PEGDA), and as a multimaterial structure combining PEGDA with 3D-printed PCL scaffolds (Fig. 17). The authors’ results demonstrated that the hydrogel PEGDA as a core in the scaffold mimics more proximately the mechanical properties of the native tissue (Fig. 18). More recently, 3D-tailored TMJ disc implants were developed and implanted in black Merino sheep:
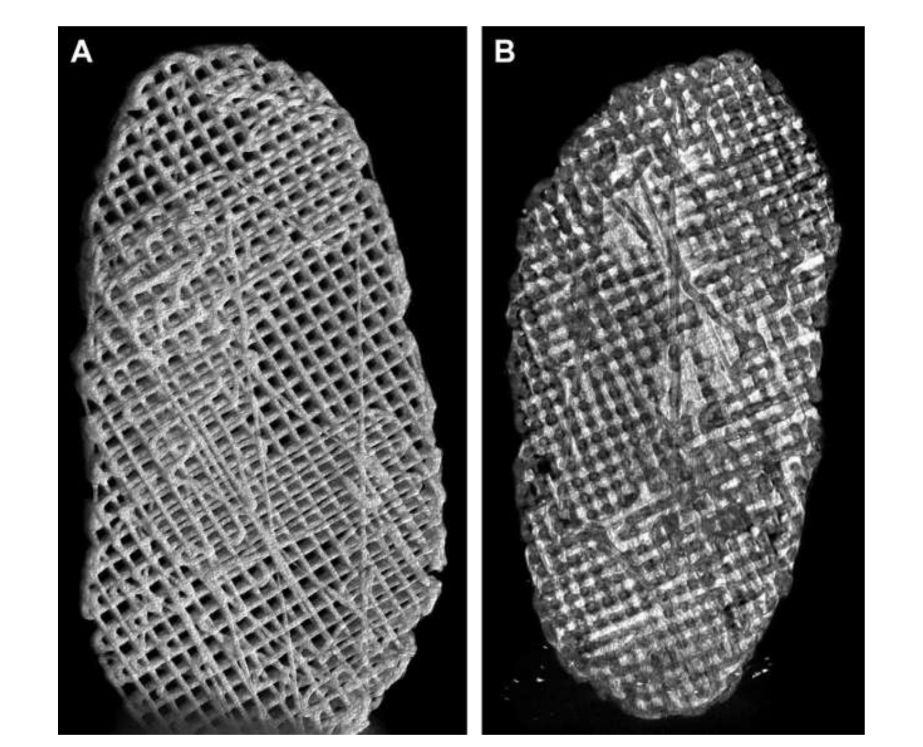
(1) Poly(glycerol sebacate) (PGS) scaffold reinforced with electrospun PCL fibers on the outer surface (PGS + PCL); (2) PCL and PEGDA (PCL + PEGDA); and (3) PCL (Figs. 19 and 20). The results showed that PCL and PCL + PEGDA discs presented a higher risk to increase degenerative changes, owing to material fragmentation. None of the tested discs regenerate a new autologous disc; however, PGS + PCL was safe, demonstrated rapid resorption, and was capable of preventing condyle degenerative changes. Hagandora in an in vitro study also pointed out a great property of PGS taking account that fibrochondrocytes respond to the application of mechanical forces by producing elevated amounts of extracellular matrix.
Despite the research that has been on-going in recent years, a biomaterial that meets all the necessary characteristics to replace the TMJ disc is still not yet available for clinical trial. It is expected that in the next few years this will become possible.
Another important branch of TE research is in the multipotent cells. Among these cells, the mesenchymal stem cells (MSCs) are the most studied, especially in TMD osteoarthritis (OA) treatment. Derived from a variety of tissues, including bone, adipose, and synovium, MSCs possess multiple properties: chondrogenic differentiation, anti-inflammatory activity, fibrocartilage regeneration, and osteogenic differentiation. Despite some promising results in the protection of OA and condylar resorption, the studies are mainly based on intraarticular injections. The use of these cells in the regeneration of the articular disc is scarcer and is mainly used with other biomaterials. In rabbits, Ahtiainen and colleagues designed a PLA disc with adipose stem cells and observed that these cells improved the morphologic pattern of bone, more similar to the native, and was observed as regeneration of the adjacent tissue. More recently, a study using adipose-derived stem cells was designed to differentiate these cells in TMJ disc cells through laser induction. More than 90% of the cells were viable with fibroblastic and chondrogenic phenotypes. The application of this approach has not been applied in in vivo trials. In a pilot study, using fibrin/chitosan hybrid scaffolds with synovium-derived MSCs, the investigators observed regenerative ability and overexpression in rats with TMJ disc perforated. Dental pulp stem cells were also used in chitosan/alginate scaffolds and evaluated in in vitro culture. These stem cells showed increased storage modulus and elastic properties, increasing the cells’ adhesion and the expression of fibrocartilaginous markers. However, its effectiveness in in vivo trials remains to be demonstrated. Also, multipotent mesenchymal stromal cells are identified and isolated from TMJ discs and showed proliferation and differentiation capabilities. In the near future, studies with these cells are expected to show the effectiveness in the regeneration of the TMJ disc.
To improve the properties shown with stem cells and scaffolds, some growth factors have been studied with the objective of improving the differentiation, proliferation, GAG, and collagen production. The most noticeable growth factors include vascular endothelial growth factor, bone morphogenetic protein-2, fibroblast growth factor (FGF), TGF-b1, high mobility group 1 protein, insulin growth factor-1 (IGF- 1); platelet-derived growth factor, epidermal growth factor, interleukin 1, and tumor necrosis factor-alpha. In literature, some investigators explored the potential of embedding these growth factors in different scaffolds. Detamore and Athanasiou were pioneers incorporating 3 growth factors (FGF, TGF-b, and IGF) in PGA scaffolds. All growth factors improved mechanical and structural integrity; however, IGF and TGF-b were most effective at promoting collagen synthesis. In PLLA scaffolds treated with IGF1 or TGF-b1 or TGF-b3, the results were better, with TGF-b1 promoting a larger number of cells, collagen, and glycosaminoglycans. PCL was also encapsulated with microspheres of CTGF and TGFb3. When cultured with human mesenchymal stem/progenitor cells, this scaffold was efficient in generating heterogeneous fibrocartilaginous matrix, and viscoelastic properties. In the future, it is expected to be able to explore this concept incorporating the biomaterials with stem cells and growth factors; however, bureaucratic and ethical constraints must be reviewed to reinforce the expectation to use this techniques in humans.
Summary
The demand for a TMJ disc replacement continues to represent a major challenge today. The great difficulty continues to be to develop a biomaterial that has the biomechanical and biochemical properties to represent a viable alternative.
The TE field has actively contributed to the possibility of bringing new outcomes to the search for a new and long-lasting tissue that effectively substitutes/regenerates the TMJ disc. Studies should take in consideration the native properties of the disc, such as mechanical, physical, and biological. A standardization of studies in large animals such as sheep and pigs should be also applied.
Although it has not yet been possible to achieve an ideal biomaterial, the work developed in recent years makes it possible that this goal is closer.
David Faustino Ângelo, Florencio Monje Gil
References
- Herring SW. TMJ anatomy and animal models. J Musculoskelet neuronal interactions 2003;3(4):391-407.
- Naples VL. Morphology, evolution and function of feeding in the giant anteater (Myrmecophaga tridactyla). J Zool 1999;249(1): 19-41.
- Lee YK, Moon HJ. Reciprocal influence of masticatory apparatus, craniofacial structure and whole body homeostasis. Med Hypotheses 2012;79(6):761-6.
- Herring SW, Liu ZJ. Loading of the temporomandibular joint: anatomical and in vivo evidence from the bones. Cells Tissues Organs 2001;169(3):193-200.
- Bosanquet A, Ishimaru J, Goss AN. Effect of experimental disc perforation in sheep temporomandibular joints. Int J Oral Maxill Surg 1991;20(3):177-81.
- Bosanquet AG, Goss AN. The sheep as a model for temporomandibular joint surgery. Int J Oral Maxill Surg 1987;16(5):600-3.
- Ishimaru J-I, Goss AN. A model for osteoarthritis of the temporomandibular joint. J Oral Maxillofacial Surg 1992;50(11):1191-5.
- Long X, Goss AN. A sheep model of intracapsular condylar fracture. J Oral Maxillofac Surg 2007;65(6):1102-8.
- Helgeland E, Shanbhag S, Pedersen TO, et al. Scaffold-based temporomandibular joint tissue regeneration in experimental animal models: a systematic review. Tissue Eng B Rev 2018;24(4): 300-16.
- Wang KH, Chan WP, Chiu LH, et al. Histological and Immunohistochemical Analyses of repair of the disc in the rabbit temporomandibular joint using a collagen Template. Materials (Basel) 2017; 10(8).
- Sharawy MM, Helmy ES, Bays RA, et al. Repair of temporomandibular joint disc perforation using a synovial membrane flap in Macaca fascicularis monkeys: light and electron microscopy studies. J Oral Maxillofac Surg 1994;52(3):259-70.
- Ali AM, Sharawy MM. Histopathological changes in rabbit craniomandibular joint associated with experimentally induced anterior disk displacement (ADD). J Oral Pathol Med 1994;23(8): 364-74.
- Mills DK, Daniel JC, Herzog S, et al. An animal model for studying mechanisms in human temporomandibular joint disc derangement. J Oral Maxillofac Surg 1994;52(12):1279-92.
- Tallents RH, Macher DJ, Rivoli P, et al. Animal model for disk displacement. J Craniomandib Disord 1990;4(4):233-40.
- Legrell PE, Isberg A. Mandibular height asymmetry following experimentally induced temporomandibular joint disk displacement in rabbits. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;86(3):280-5.
- Sindelar BJ, Herring SW. Soft tissue mechanics of the temporomandibular joint. Cells Tissues Organs 2005;180(1):36-43.
- Sun Z, Liu ZJ, Herring SW. Movement of temporomandibular joint tissues during mastication and passive manipulation in miniature pigs. Arch Oral Biol 2002;47(4):293-305.
- Herring SW, Decker JD, Liu ZJ, et al. Temporomandibular joint in miniature pigs: anatomy, cell replication, and relation to loading. Anat Rec 2002;266(3):152-66.
- Liu ZJ, Herring SW. Masticatory strains on osseous and ligamentous components of the temporomandibular joint in miniature pigs. J Orofac Pain 2000;14(4):265-78.
- Sindelar BJ, Evanko SP, Alonzo T, et al. Effects of intraoral splint wear on proteoglycans in the temporomandibular joint disc. Arch Biochem Biophys 2000;379(1):64-70.
- Vapniarsky N, Aryaei A, Arzi B, et al. The Yucatan minipig temporomandibular joint disc structure-function Relationships Support its Suitability for human Comparative studies. Tissue Eng C Methods 2017;23(11):700-9.
- Thoma KH. Hyperostosis of the mandibular condyle: with report of two cases. Am J Orthod Oral Surg 1945;31(10):597-607.
- Angelo DF, Morouc‚o P, Alves N, et al. Choosing sheep (Ovis aries) as animal model for temporomandibular joint research: morphological, histological and biomechanical characterization of the joint disc. Morphologie 2016;100(331):223-33.
- Ângelo DF, Monje FG, González-García R, et al. Bioengineered temporomandibular joint disk implants: study protocol for a two-phase Exploratory randomized preclinical pilot trial in 18 black Merino sheep (TEMPOJIMS). JMIR Res Protoc 2017;6(3):e37.
- Herring SW. TMJ anatomy and animal models. J Musculoskelet Neuronal Interactions 2003;3(4):391-4.
- De Meurechy N, Mommaerts M. Alloplastic temporomandibular joint replacement systems: a systematic review of their history. Int J Oral Maxill Surg 2018;47.
- Ângelo DF, Morouc‚o P, Monje Gil F, et al. Preclinical randomized controlled trial of bilateral discectomy versus bilateral discopexy in black Merino sheep temporomandibular joint: TEMPOJIMS - phase 1-histologic, imaging and body weight results. J Craniomaxillofac Surg 2018;46(4):688-96.
- Cohen WA, Servais JM, Polur I, et al. Articular cartilage degeneration in the contralateral non-surgical temporomandibular joint in mice with a unilateral partial discectomy. J Oral Pathol Med 2014; 43(2):162-5.
- Ahtiainen K, Mauno J, Ellä V, et al. Autologous adipose stem cells and polylactide discs in the replacement of the rabbit temporomandibular joint disc. J R Soc Interf 2013;10(85):20130287.
- Bjørnland T, Haanaes HR. Discectomy of the temporomandibular joint: an experimental study in monkeys. J Craniomaxillofac Surg 1999;27(2):113-6.
- Li L, Wang L, Sun Y, et al. Establishment and histological evaluation of a goat traumatic temporomandibular joint model. J Oral Maxillofac Surg 2015;73(5):943-50.
- Xu L, Polur I, Lim C, et al. Early-onset osteoarthritis of mouse temporomandibular joint induced by partial discectomy. Osteoarthritis Cartil 2009;17(7):917-22.
- Dimitroulis G, Slavin J. The effects of unilateral discectomy and condylectomy on the contralateral intact rabbit craniomandibular joint. J Oral Maxillofac Surg 2006;64(8):1261-6.
- Ângelo DF, Gil FM, González-García R, et al. Effects of bilateral discectomy and bilateral discopexy on black Merino sheep rumination kinematics: TEMPOJIMS - phase 1 - pilot blinded, randomized preclinical study. J Craniomaxillofac Surg 2018;46(2):346-55.
- Yaillen DM, Shapiro PA, Luschei ES, et al. Temporomandibular joint meniscectomy–effects on joint structure and masticatory function in Macaca fascicularis. J Maxillofac Surg 1979;7(4):255-64.
- Boman KA. Temporomandibular joint arthrosis and its treatment by extirpation of the disk: a clinical study. University of Michigan: Almqvist & Wiksell; 1947.
- Tolvanen M, Oikarinen VJ, Wolf J. A 30-year follow-up study of temporomandibular joint meniscectomies: a report on five patients. Br J Oral Maxill Surg 1988;26(4):311-6.
- Eriksson L, Westesson PL. Discectomy as an effective treatment for painful temporomandibular joint internal derangement: a 5-year clinical and radiographic follow-up. J Oral Maxillofac Surg 2001; 59(7):750-8.
- Bjørnland T, Larheim TA. Discectomy of the temporomandibular joint: 3-year follow-up as a predictor of the 10-year outcome. J Oral Maxillofac Surg 2003;61(1):55-60.
- Hartman LC, Bessette RW, Baier RE, et al. Silicone rubber temporomandibular joint (TMJ) meniscal replacements: Postimplant histopathologic and material evaluation. J Biomed Mater Res 1988;22(6):475-84.
- Henry CH, Wolford LM. Treatment outcomes for temporomandibular joint reconstruction after Proplast-Teflon implant failure. J Oral Maxillofacial Surg 1993;51(4):352-8.
- Tucker MR, Burkes EJ Jr. Temporary silastic implantation following discectomy in the primate temporomandibular joint. J Oral Maxillofacial Surg 1989;47(12):1290-5.
- Bosanquet AG, Ishimaru J, Goss AN. The effect of Silastic replacement following discectomy in sheep temporomandibular joints. J Oral Maxillofac Surg 1991;49(11):1204-9.
- Sanders B, Buoncristiani RD, Johnson L. Silicone rubber fossa implant removal via partial arthrotomy followed by arthroscopic examination of the internal surface of the fibrous capsule. Oral Surg Oral Med Oral Pathol 1990;70(3):369-71.
- Bavarian R, Schatman ME, Keith DA. Persistent pain following Proplast-Teflon implants of the temporomandibular joint: a case report and 35-year Management Perspective. J Pain Res 2021;14: 3033-46.
- Heffez L, Mafee MF, Rosenberg H, et al. CT evaluation of TMJ disc replacement with a Proplast-Teflon laminate. J Oral Maxillofacial Surg 1987;45(8):657-65.
- Wu Y, Gong Z, Li J, et al. The pilot study of fibrin with temporomandibular joint derived synovial stem cells in repairing TMJ disc perforation. Biomed Res Int 2014;2014:454021.
- Kobayashi E, Nakahara T, Inoue M, et al. Experimental study on in situ tissue engineering of the temporomandibular joint disc using autologous bone marrow and collagen sponge scaffold. J Hard Tissue Biol 2015;24:211-8.
- Almarza AJ, Athanasiou KA. Seeding techniques and scaffolding choice for tissue engineering of the temporomandibular joint disk. Tissue Eng 2004;10(11-12):1787-95.
- Juran CM, Dolwick MF, McFetridge PS. Engineered microporosity: enhancing the early regenerative potential of decellularized temporomandibular joint discs. Tissue Eng A 2015;21(3-4): 829-39.
- Matuska AM, McFetridge PS. Laser micro-ablation of fibrocartilage tissue: effects of tissue processing on porosity modification and mechanics. J Biomed Mater Res B Appl Biomater 2018;106(5): 1858-68.
- Liang J, Yi P, Wang X, et al. Acellular matrix hydrogel for repair of the temporomandibular joint disc. J Biomed Mater Res B Appl Biomater 2020;108(7):2995-3007.
- Mäenpää K, Ellä V, Mauno J, et al. Use of adipose stem cells and polylactide discs for tissue engineering of the temporomandibular joint disc. J R Soc Interf 2010;7(42):177-88.
- Detamore MS, Athanasiou KA. Use of a rotating bioreactor toward tissue engineering the temporomandibular joint disc. Tissue Eng 2005;11(7e8):1188-97.
- Allen KD, Athanasiou KA. Scaffold and growth factor selection in temporomandibular joint disc engineering. J dental Res 2008; 87(2):180-5.
- Legemate K, Tarafder S, Jun Y, et al. Engineering human TMJ discs with protein-Releasing 3D-printed scaffolds. J dental Res 2016; 95(7):800-7.
- Jiang N, Yang Y, Zhang L, et al. 3D-Printed Polycaprolactone reinforced hydrogel as an Artificial TMJ disc. J dental Res 2021; 100(8):839-46.
- Moura C, Trindade D, Vieira M, et al. Multi-material implants for temporomandibular joint disc repair: tailored additive Manufacturing production. Front Bioeng Biotechnol 2020;8:342.
- Ângelo DF, Wang Y, Morouc‚o P, et al. A randomized controlled preclinical trial on 3 interposal temporomandibular joint disc implants: TEMPOJIMS-Phase 2. J Tissue Eng regenerative Med 2021; 15(10):852-68.
- Hagandora CK, Gao J, Wang Y, et al. Poly (glycerol sebacate): a novel scaffold material for temporomandibular joint disc engineering. Tissue Eng Part A 2013;19(5e6):729-37.

/social-network-service/media/default/6809/fbab08d0.jpg)