Injectable silicone-based gingival mask technique: Transferring the emergence profile of multiple implant restorations
Interim implant-supported restorations play an important role in achieving the desired esthetic outcome and long-term success of implant prostheses. The initial interim restoration is made from a conventional implant-level impression, which is then modified to sculpt the gingival contour. Additional material is added to mold the papillae and gingival margins and recreate the natural gingival architecture. An appropriate impression technique is essential for an accurate transfer of the peri-implant emergence profile to the definitive cast.
Two different techniques have been described to transfer the emergence profile from the patient’s mouth to the definitive cast. More details about restorations in the Kois concept on Tak On Tse Ryan course.
The indirect technique uses a custom impression coping to copy the peri-implantitis emergence profile. A standard impression coping is modified by filling the space with autopolymerizing or light-polymerizing resin between the impression copings and the submarginal emergence profile as outlined by a silicone matrix. This technique can transfer the emergence profile from the patient’s mouth to the definitive cast with high precision. However, the technique is time-consuming and only suitable for a single implant. For multiple implant restorations with pontic site development, this technique is complex, as the subgingival emergence profile of several implant abutments and the pontic area need to be replicated. The custom impression copings must be splinted to accurately transfer the position of the implants. A disadvantage of the indirect technique is that the peri-implant soft tissue will collapse during the fabrication of the indirect custom impression copings. When the interim restoration is delivered, the patient will feel discomfort as the tissue is displaced. Schoenbaum and Han10 described an efficient and accurate direct custom implant impression coping technique to transfer the emergence profile of an implant abutment and pontic site to the definitive cast. However, this technique is limited to restorations supported by 2 implants. A concern has been expressed that the heat generated by the flowable composite resin and its toxicity may damage the gingival tissue.11 The injectable silicone-based gingival mask technique was developed to transfer the peri-implant emergence profile and the gingival margin of the interim restoration to the definitive cast.
Technique
Use an implant-level impression, splinting the impression copings, to fabricate a soft tissue cast (Fig. 1).
Direct the dental laboratory to fabricate an interim restoration replicating the soft tissue profile of the healing abutments (Fig. 2).
Modify the emergence profile and pontic area of the interim restoration with flowable composite resin (Filtek; 3M ESPE) (Fig. 3).
Reappoint the patient after 6 weeks to allow tissue maturation (Fig. 4).
Make an intraoral impression of the maxilla using an irreversible hydrocolloid (Jeltrate; Dentsply Sirona) to record the interim restoration with the gingival margin and soft tissue profile.
Fabricate a vacuum-formed matrix from a clear, hard thermoplastic sheet (Pro-form 0.020 temp splint; Keystone Industries) to cover the gingival tissue and prepare a small hole in the gingival area (Fig. 5).
Remove the interim restoration and replace it on the definitive cast without the original gingival mask (Figs. 6, 7).
Seat the vacuum-formed matrix over the interim restoration on the definitive cast (Fig. 8).
Inject the gingival mask material (Muller; Omicron GmbH & Co KG) directly around the implant replicas and into the space under the pontic through the hole in the vacuum-formed matrix (Figs. 9-11).
Alternatively, to ensure that there are no air bubbles in the critical areas, the gingival mask material may be injected directly around the abutments and under the pontics before seating the vacuum-formed matrix. Then seat the matrix and continue to inject through the hole in the matrix until excess flows out under the matrix.
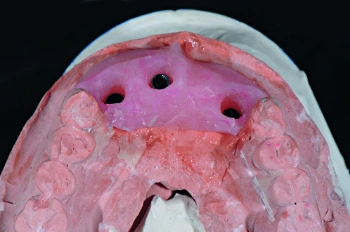 Figure 1. Soft tissue working cast made from original implant impression using splinted impression copings. Gingival contour represent shape of healing abutments.
Figure 1. Soft tissue working cast made from original implant impression using splinted impression copings. Gingival contour represent shape of healing abutments.
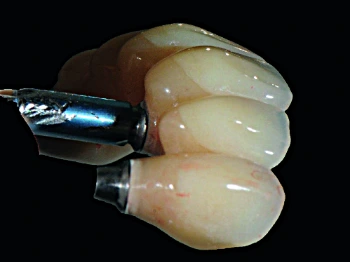 Figure 2. Interim restoration as fabricated by dental laboratory technician.
Figure 2. Interim restoration as fabricated by dental laboratory technician.
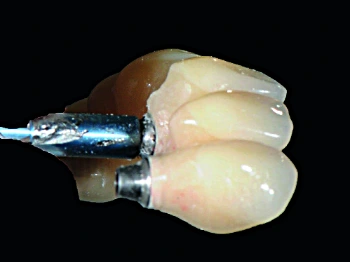 Figure 3. Interim restoration as modified by treating dentist for ideal emergence profile and ovate pontic contour.
Figure 3. Interim restoration as modified by treating dentist for ideal emergence profile and ovate pontic contour.
 Figure 4. Tissue condition after 6-week maturation period.
Figure 4. Tissue condition after 6-week maturation period.
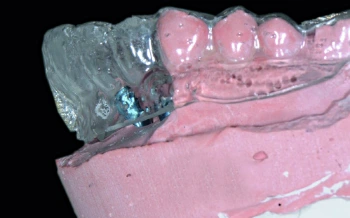 Figure 5. Vacuum-formed clear matrix with hole placed for injection of silicone-based gingival mask.
Figure 5. Vacuum-formed clear matrix with hole placed for injection of silicone-based gingival mask.
 Figure 6. Interim restoration removed. Note tissue sculpted to desired architecture.
Figure 6. Interim restoration removed. Note tissue sculpted to desired architecture.
 Figure 7. Interim restoration fastened to original definitive cast.
Figure 7. Interim restoration fastened to original definitive cast.
 Figure 8. Vacuum-formed clear matrix placed on original definitive cast with interim restoration attached.
Figure 8. Vacuum-formed clear matrix placed on original definitive cast with interim restoration attached.
 Figure 9. Silicone-based gingival mask material injected into space between definitive cast, clear vacuum-formed matrix, and interim restoration.
Figure 9. Silicone-based gingival mask material injected into space between definitive cast, clear vacuum-formed matrix, and interim restoration.
 Figure 10. Original definitive cast modified with gingival mask.
Figure 10. Original definitive cast modified with gingival mask.
 Figure 11. Gingival mask capturing emergence profile of abutments and contour of pontic sites, eliminating need for second impression.
Figure 11. Gingival mask capturing emergence profile of abutments and contour of pontic sites, eliminating need for second impression.
Summary
The injectable gingival mask material can transfer the emergence profile of implant abutments and the pontic site to the definitive cast both accurately and precisely. It is a straightforward technique that saves chairside time and does not require an additional impression. The clinician can modify the emergence profile and mold the papillae to optimize the access for hygiene and esthetics; this is then accurately transferred to the definitive cast. This technique can be used in different clinical situations, including different implant angulations.
References
Kois JC, Kan JY. Predictable peri-implant gingival aesthetics: surgical and prosthodontics rationales. Pract Proced Aesthet Dent 2001;13: 691-8.
Garber DA. The esthetic dental implant: letting the restoration be the guide. J Am Dent Assoc 1995;126:319-25.
Lazzara RJ, Porter SS. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent 2006;26:9-17.
Drago C, Lazzara RJ. Guidelines for implant abutment selection for partially edentulous patients. Compend Contin Educ Dent 2010;31:14-20.
Chee WWL, Cho GC, Ha S. Replicating soft tissue contours on working casts for implant restorations. J Prosthodont 1997;6:218-20.
Elian N, Tabourian G, Jalbout ZN, Classi A, Cho SC, Froum S, et al. Accurate transfer of peri-implant soft tissue emergence profile from the provisional crown to the final prosthesis using an emergence profile cast. J Esthet Restor Dent 2007;19:306-14.
Chee W, Jivraj S. Impression techniques for implant dentistry. Br Dent J 2006;201:429-32.
Shor A, Schuler R, Goto Y. Indirect implant-supported fixed provisional restoration in the esthetic zone: fabrication technique and treatment work-flow. J Esthet Restor Dent 2008;20:82-95.
den Hartog L, Raghoebar GM, Stellingsma K, Meijer HJA. Immediate loading and customized restoration of a single implant in the maxillary esthetic zone: a clinical report. J Prosthet Dent 2009;102:211-5.
Schoenbaum TR, Han TJ. Direct custom implant impression copings for the preservation of the pontic receptor site architecture. J Prosthet Dent 2012;107:203-6.
Tadin A, Marovic D, Galic N, Kovacic I, Zeljezic D. Composite-induced toxicity in human gingival and pulp fibroblast cells. Acta Odontol Scand 2014;72:304-11.
Esguerra RJ. Technique for fabricating a custom gingival mask using a maxillary complete-arch implant-supported fixed interim prosthesis with an integrated verification cast. J Prosthet Dent 2016;115:5-8.
/social-network-service/media/default/37635/9f9c3bb2.jpg)