Immediate implantation using the extracted crown
Машинний переклад
Оригінальна стаття написана мовою RU (посилання для прочитання).
Statement of the problem: It has previously been shown that immediate implantation into fresh sockets is a predictable treatment method for restoring non-restorable teeth in the anterior areas of the upper jaw.
About the risks and complications of immediate implantation in an aesthetically significant area at the webinar Immediate implantation in an aesthetic area .
Purpose: This article reports a clinical case in which an immediate implant placement protocol was used in combination with two separate and sequential grafts (bovine bone and connective tissue), followed by direct implantation using a patient crown from an extracted tooth.
Clinical report: Physical, clinical and external examination of the patient (female, 23 years old) showed that the maxillary central incisor (tooth number 8) has little mobility due to the presence of extensive resorption in the cervical area.
Results: Using the crown of an extracted tooth as a temporary crown after immediate implant placement resulted in rapid achievement of an aesthetically pleasing result and long-term favorable results.
Conclusion: The proposed treatment protocol can be effectively used to directly restore patient esthetics and function while maintaining gingival tissue health, volume, and contour over a 12-month follow-up period.
Clinical relevance: Extraction of anterior teeth usually requires the fabrication of single-piece dentures using synthetic materials (such as polymers), which often fail to achieve the esthetic and physiological results expected by patients. The use of the patient's own crown has been demonstrated to achieve good clinical results and preserve the natural shape and function of the tissue.
Immediate implantation
The field of dental implantology has changed significantly over the past few years. Major improvements include the development of new materials, technologies and equipment, which together have made immediate implantation (immediate, early) a viable and predictable treatment option with long-term success rates ranging from 90% to 100%. Although this strategy has some important advantages over traditional implant placement protocols, such as time efficiency, immediate esthetics, and improved patient comfort, direct implant placement cannot prevent hard and soft tissue remodeling. Therefore, it is considered a risky procedure by some researchers and clinicians. However, immediate implantation and placement of temporary structures have been used in many patients.
Bruno et al., studying the specific location of the contact zones of temporary crowns in the area of the interproximal papillae, showed that the use of direct treatment methods resulted in the interdental papillae and dental implants being largely preserved. This was associated with less soft tissue remodeling while maintaining gingival level.
Esposito et al., Schropp and Isidor systematically reviewed the literature regarding the use of immediate placement of implants in fresh extraction sockets and concluded that this treatment has merit. It can provide better aesthetic results and higher levels of patient satisfaction compared to delayed implant placement methods. The authors also stated that immediate implant placement procedures are technique sensitive and more difficult to perform than conventional procedures. Thus, they suggested that direct techniques should be performed by a well-trained dental team.
Due to the high demands of patients on aesthetics in the smile zone, restoration of extracted maxillary incisors is now considered the main indication for the use of immediate implant placement procedures. Becker et al studied immediate pre-placement of single-tooth implants (5.8 mm or larger) in fresh sockets. They found that pre-insertion of implants is a favorable and predictable treatment option if certain minimum criteria are met (eg, insertion torque = 15 Ncm, insertion stability factor = 50, apical bone amount = 3 mm). Achieving primary stability is now considered the cornerstone of direct treatment modalities. This is an important factor in achieving long-term favorable and aesthetic results.
Other factors such as precise implant positioning and prosthetic use have also been associated with healing and soft tissue preservation in immediate/temporary placement. Malchiodi et al examined the relationship between the interproximal alveolar ridge and soft tissue and its impact on long-term aesthetic outcomes (3-year follow-up). According to their findings, there is a strong relationship between hard and soft tissues, where maintaining tissue architecture (at the surgical site) is key to achieving long-term optimal aesthetic results. In this case, if the bone support is insufficient or its thin biotype is detected before surgery, then a transplantation procedure (in particular connective tissue) is necessary to maintain and stabilize the periodontal tissues.
In a clinical and radiographic cohort study by Pozzi and Mura, results showed that direct use of implants with a conical body and an internal moving platform (NobelReplace Conical Connection, Nobel Biocare, nobelbiocare.com) contributed to the maintenance of marginal bone ridge and surrounding tissue esthetics in both the socket and and in healthy bone. Therefore, the primary purpose of this study is to describe a clinical procedure in which a method based on direct implant and graft (bovine bone and connective tissue) placement was used to restore an extracted maxillary incisor with external resorption.
Clinical case
A 23-year-old female patient received dental care at the endodontic clinic at Positivo University (Curitiba, PR, Brazil). The maxillary central incisor was assessed. The patient's main complaint was slight tooth mobility, which was caused by an injury that occurred 10 years ago. The medical history revealed that there were no symptoms of pain at the time of injury or in subsequent years.

Picture 1
Clinical examination
The patient's medical and dental history excluded any contraindications (eg, uncontrolled heart disease or diabetes mellitus) for dental procedures. A general and detailed clinical examination revealed a tooth with preserved anatomy and color and surrounding healthy periodontal tissue (i.e., no pockets or bleeding were detected on probing).
The vital test resulted in a negative response to the cold stimulus (-50C, Endo-Ice, Maquira, maquira.com.br). Cone beam computed tomography (CBCT) (field of view 5 × 5, 0.14, 25 seconds) (PreXion3D, PreXion, prexion.com) was performed to further evaluate the periapical bone tissue (Figs. 1 and 2) and revealed the presence of extensive external resorption of the neck of the tooth (NRShz) with the support of interproximal bone ridges.
Based on the latest classification of NRS3 proposed by the European Society of Endodontology and the American Academy of Oral and Maxillofacial Radiology, Patel et al classified the NRS3 observed in this study as 3BP (where "3" means that the height of the lesion extends to the middle third of the root, "B" " means >90 – 180 degrees, and "P" indicates probable endodontic involvement).
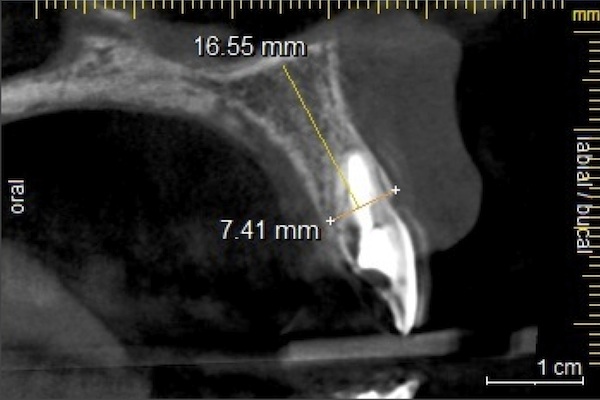
Figure 2
Patient Treatment Plan
The proposed treatment plan consisted of atraumatic tooth extraction followed by immediate placement of an implant, together with a bone graft (bovine bone) to fill the gap and a subepithelial connective tissue graft to stabilize the periodontal soft tissue. Restorative procedures included immediate pre-implantation using an extracted clinical crown adapted as a temporary crown. The rationale for the proposed treatment plan was to ensure that the patient's aesthetics were maintained while restoring function to the lost element.
Surgical treatment procedures
Surgical procedures were performed under local infiltration anesthesia (articaine 4% with epinephrine [ 1:100,000 ] ), the needle was inserted vestibularly and palatally. An internal incision was made from the distal surface of the adjacent tooth, thereby creating a flap that would allow visual assessment of the area affected by the HRS (Figure 3). Atraumatic removal was performed using a scalpel (n # 15c, SOLIDOR®, solidor.com.br) to preserve the majority of periodontal structures.

Figure 3
A tapered tapered implant (MT, length 3.5 mm x 11.5 mm, Neodent, instradent.us) was placed 3 mm apical to the gingival margin (per manufacturer's instructions) at the prepared surgical site. The establishment of primary stability was confirmed by a torque wrench, which indicated the presence of a torque of 30 N*cm. A 1-mm thick bovine implant (Lumina-Bone, Critéria, criteria.com.br) was then placed between the implant and the buccal bone plate to fill each gap present, while a second graft (from harvested connective tissue) was placed ) over the first graft to serve as a biological barrier during the healing process and to increase gingival volume (Figure 4). The vertical suture was performed using nylon suture (5-0, Ethicon, Johnson & Johnson, ethicon.com).

Figure 4
The selected clinical crown was then separated from the root, prepared and adjusted to fit the prosthetic implant abutment. It was cemented using a light-curing composite (shade A2, Empress® Direct, Ivoclar Vivadent, ivoclarvivadent.com). The adapted crown was screwed into the implant and occlusal adjustments were made to avoid super-contacts (central, lateral and anterior) (Fig. 5).

Figure 5
Postoperative condition
The patient was prescribed a broad-spectrum antibiotic (amoxicillin, 500 mg, every 8 hours, 7 days), an anti-inflammatory drug (nimesulide, 100 mg, every 12 hours, 3 days) and an analgesic (paracetamol, 750 mg, every 8 hours, 3 days) . Postoperative oral hygiene instructions were given to the patient before discharge, and sutures were removed 10 days after surgery.
A follow-up clinical appointment 30 days later showed that a satisfactory short-term aesthetic result had been achieved. After 90 days and 12 months at follow-up clinical appointments, there was a significant improvement in periodontal health with maintenance of gingival volume, increasing profile and interproximal bone ridge, which together contributed to the achievement of gingival esthetics (Figure 6). (Author's note: Rationale for presenting the 12-month follow-up x-ray: The author's CT device was not available at the time, so the 12-month CT is not available).

Figure 6

Figure 7
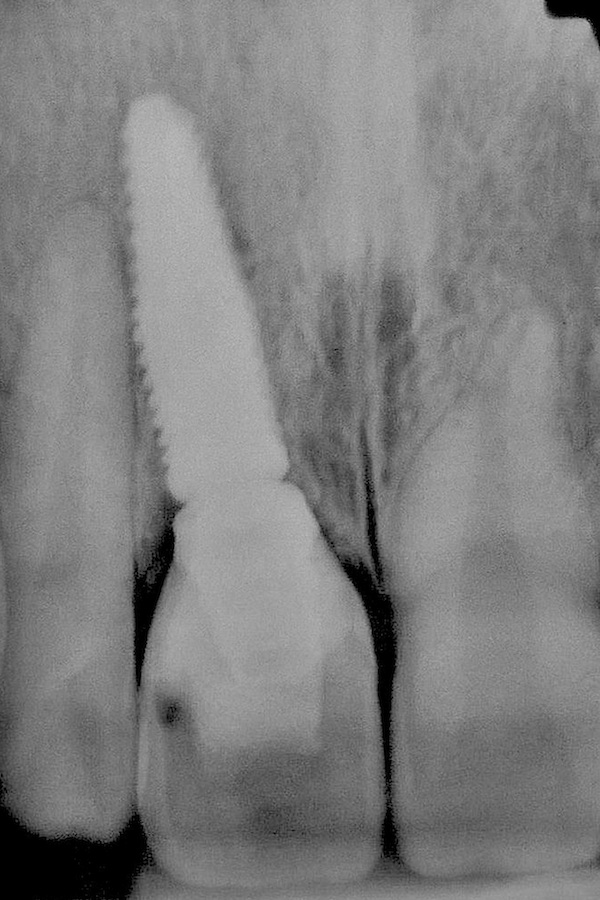
Figure 8
Restoration of the maxillary central incisor
The purpose of this case report was to describe the restoration of a maxillary central incisor affected by severe NRS. The proposed treatment plan included an immediate implant placement protocol followed by immediate pre-implantation using the crown of the patient's extracted tooth. The treatment plan resulted in immediate aesthetic results for the patient while maintaining the natural contours of the gums and gingival papillae.
The results presented here show that the chosen surgical treatment protocol allowed for correct placement of the implant while ensuring primary stability, as evidenced by torque values (30 Ncm). Using the patient's clinical crown for implantation provided the surrounding tissues with ideal physiological distances between the contact points and the alveolar bone ridge, resulting in periodontal tissues that are well supported and adaptable.
Together, these factors led to optimal gingival aesthetics and minimal disruption to the patient's psychological state in the short and long term. Periodontal biotypic evaluation is fundamental to the success of implants placed using the methods described here. Proper selection and use of biomaterials for gap filling and guided tissue regeneration are critical to achieving sufficient support for both hard and soft tissues. Although the patient's buccal bone plate and gingival tissue were extremely thin, the types of biomaterials used in combination with the placement technique maintained tissue architecture and prevented tissue remodeling and subsequent tissue shrinkage. The results indicate that the use of a tapered implant is a factor in maintaining the gingival bone and improving the esthetics of the adjacent gingival tissues during a 12-month follow-up.
Immediate dental implantation (Conclusions)
The present case demonstrated the usefulness of a protocol of immediate dental implantation followed by immediate pre-use of the patient's own crown. The results obtained clearly show that the treatment protocol used resulted in long-term preservation of gingival contour and volume. The use of biomaterials along with direct placement of the patient's crown has proven to be a feasible treatment option.
Learn more about the effectiveness and protocol for immediate implantation at the webinar Immediate one-step implantation .
http://www.aegisdentalnetwork.com/

