Dental Plaque Microorganisms
Машинний переклад
Оригінальна стаття написана мовою RU (посилання для прочитання) .
As of today, microbiologists have made significant progress in studying the role of bacterial flora in dental plaque in the development of periodontal diseases.
About the study of the oral microbiota at the webinar on oral microbiota at the webinar Cariesology: diagnostics, risk assessment, non-invasive and minimally invasive treatment in pediatric dentistry.
Dental Plaque
Several hours after thorough tooth brushing, dental plaque begins to form again on the teeth due to certain physicochemical processes between the enamel surface and saliva components, resulting in the formation of the thinnest film — the pellicle.
The process of its formation undergoes the following stages:
- bacterial migration,
- adhesion,
- attachment,
- colonization.
Microbial associations constantly grow against the backdrop of insufficient hygienic care. After 36 hours, dental plaque, which is a structured, soft formation attached to the tooth and cannot be washed off with water, is visually determined during a clinical examination.

Figure 1. Microorganisms of dental plaque.
The intensity of dental plaque formation is conditioned by several factors, among which are:
- daily habits (frequency of eating, smoking, quality of hygiene, use of fluorides, antibacterial drugs),
- biochemical and biophysical indicators of oral fluid,
- structural features of teeth,
- retention factors,
- features of the bite.
Dental plaque that remains on the tooth surface for a long time gradually mineralizes, forming tartar. Calcification is the result of the complex influence of bacterial, biological, and physicochemical factors. As a result of the penetration of calcium phosphate crystals from saliva, these begin to deposit on the colloidal base. This occurs in supragingival plaque, while in subgingival plaque, minerals come from blood serum. Mineralization of dental plaque can occur within 12 days. Complete tartar formation occurs after a month.
The growth of tartar on the tooth surface occurs due to the accumulation of a layer of dental plaque. Dental tartar, having a rough surface, predisposes to the adhesion of microorganisms. As the thickness of the plaque increases, its species microbiological composition changes.

Figure 2. Dental plaque under a microscope.
Approximately 600 varieties of bacteria have been identified that inhabit supra- and subgingival plaque. On the second to third day, the plaque predominantly includes gram-positive aerobes, mainly streptococci and actinomycetes.
The consumption of oxygen by aerobic microorganisms reduces the local redox potential, which creates conditions for the appearance of gram-negative anaerobes on the third to fourth day.
Along with changes in the microflora, there is a complex interaction between different species. For example, St. Actinomyces ferment sugars, increasing the concentration of lactic acid, which is necessary for the life of anaerobic gram-negative cocci Veillonella, and their metabolic product - menadione is necessary for the life of Prevotella intermedia and Porphyramonas gingivalis.
The metabolic products of gram-negative anaerobes create favorable conditions for further activation of anaerobic colonization. Fusobacterium nucleatum causes the accumulation of ammonium cation; members of the genus Capnocytophaga produce succinic acid anion; Campylobacter — an organic red pigment containing iron. The described metabolites support the life of other more aggressive bacteria, which have been classified by scientists as potentially periodontopathogenic. This fact underscores their significant role in the pathogenesis of periodontitis, the formation of periodontal pockets, resorption of the alveolar process, and destruction of connective tissue.
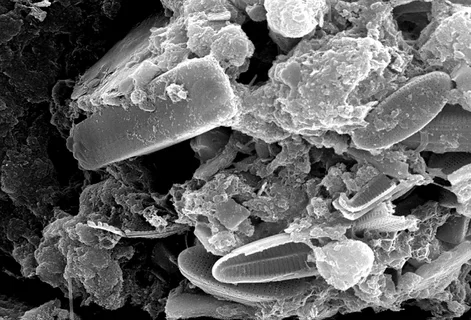
Figure 3. Microbial biofilm.
To identify the microorganisms living in the periodontal area, the following criteria were proposed for this group:
- association with disease – the strain's numbers increase at the site of the lesion as the disease progresses;
- the number of the strain decreases in the area of the lesion when effective treatment is administered;
- invasion of species representatives into the periodontal tissues causes a humoral and cellular immune response;
- presence of virulence mechanisms that can cause destruction of periodontal tissues;
- ability of the strain to become an etiological factor of periodontal disease.
Virulence of Dental Plaque Bacteria
Virulence is the ability of a microorganism to infect a given organism. It should not be confused with pathogenicity – the ability to cause disease development, since an infectious agent after infection can become a symbiont of the host. Virulence depends on the properties of the infectious agent itself – these are virulence factors and on the susceptibility, sensitivity of the host organism.
Virulence factors of dental plaque microorganisms are divided into two major groups:
- factors that allow bacteria to colonize on the tissues of the oral cavity and penetrate deeper (attachment, colonization, invasiveness);
- factors that allow microorganisms to indirectly or directly cause destruction of the host tissues (antigenicity, toxigenicity, invisibility to the immune system).
Adhesion and Colonization
The ability of an infectious agent to attach in the periodontal environment is a virulence factor. The periodontal pocket, like the gingival groove, contains gingival fluid, which moves from the base of the pocket or groove outward. Representatives of bacteria colonizing this area attach to surrounding surfaces (tooth root or crown, existing plaque, soft tissues) in such a way as to avoid being washed away by the fluid flow.
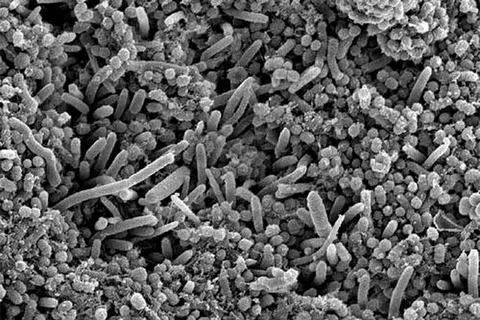
Figure 4. Colonization of the tooth surface.
The first to attach to the pellicle on the tooth surface are Streptococcus sanguis, oralis, mitis, which possess surface receptors that facilitate the subsequent attachment (coaggregation) of other bacterial species. The literature describes in detail such interactions — Actinomyces viscosus attaches to Streptococcus sanguis through surface fimbriae due to the polysaccharide receptors of the latter. Porphyromonas gingivalis attaches to fibroblasts and epithelial cells using fimbriae. P. gingivalis has the ability to connect to other bacteria, epithelial cells, and connective tissue structures, which is a virulence factor of this microorganism.
The basis of bacterial colonization lies in the ability of bacteria to attach to the tissues of the oral cavity and effectively interact with each other, which is considered the initial stage of successful bacterial invasion.
Invasiveness
Described in the literature, histological studies confirm the presence of microorganisms in the periodontal tissues of patients with progressive periodontitis and ulcerative gingivitis. In these studies, both gram-positive and gram-negative bacteria, including cocci, rods, spirochetes, and filaments, are found in the gum tissues and in close proximity to the bone tissue. The ability of bacteria to penetrate deep into the tissue is due to certain bacterial enzymes that have increased activity and diverse effects, among them:
- hyaluronidase,
- neuraminidase,
- collagenase,
- lecithinase.
Microorganisms penetrate the host's body through ulcerated areas in the attachment epithelium, observed in the intercellular space of the gums. Another method of invasion is the direct penetration of the infectious agent into the host's epithelial cells or connective tissue cells. The second method of penetration is characteristic of the following microorganisms: P. gingivalis, A. actinomycetemcomitans, Treponema denticola, and F. nucleatum.

Figure 5. Removal of dental plaque.
Researchers believe that the exacerbation of chronic inflammation of the periodontal tissues directly depends on the next phase of bacterial penetration of the periodontal tissues. The periodontal pocket acts as a reservoir of microorganisms, whose recolonization triggers a sharp spike in disease activity. This hypothesis has been clinically confirmed. In the treatment of patients diagnosed with progressive periodontitis, mechanical cleaning of the periodontal pocket alone is not enough to stabilize the inflammatory process. In affected areas, it is not possible to reduce the colonization of A. Actinomycetemcomitans, and the administration of systemic antibiotics is often prescribed, frequently in conjunction with surgical treatment.
Microbial mechanisms of penetration into host tissues include direct tissue destruction, as well as mediated, caused by the action of biological mediators due to the inflammatory process in the periodontal tissues.
About important anatomical aspects of periodontal tissues in the webinar Advanced Treatment of Periodontal Diseases.